An unusual case report of Burkholderia cepacia endophthalmitis
Huan Chen, Jing-Jia Zhang, Ying-Chun Xu, Jun-Jie Ye
1Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, China
2Department of Clinical Laboratory, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, China
Dear Editor,
I am Huan Chen from the Department of Ophthalmology,Peking Union Medical College Hospital in Beijing,China. I am writing this letter to present an unusual case of Burkholderia cepacia endophthalmitis.
Burkholderia cepacia[Burkholderia cepacian complex(Bcc)]is a group of genetically unique Gram-negative bacilli with similar phenotypes, belonging to the genus pseudomonas,which is widely found in water, soil and plants. This organism is usually found in hospital environments and medical devices, especially in liquids used in hospitals, including lavage fluid and intravenous infusion, or even disinfectant and hand sanitizer.Bccis an important pathogen associated with nosocomial infection[1-3].Bccis a rare organism of endophthalmitis, which occurs mainly among postoperative cases[4-6]. Here we report a clinical picture and treatment outcomes ofBurkholderia cepaciaendophthalmitis in a patient who had no history of ocular surgery or trauma before the onset of symptoms.
This study was approved by the Review Board of Peking Union Medical College Hospital. Written informed consent to participate and publication was obtained from the patient.
Case PresentationA 66-year-old healthy female patient was admitted to Peking Union Medical College Hospital on December 11, 2018, with complaints of blurred vision and redness in the right eye for three weeks. At the very beginning of symptom onset, she was admitted to another hospital, where the best corrected visual acuity (BCVA) was 0.1; the intraocular pressure (IOP) was 11 mm Hg; a slit lamp examination showed a severe anterior chamber reaction with cellular keratic precipitates, 2+ cells and flare; and there was diffuse injection of the conjunctiva and partial iris posterior synechia. She also had vitritis with a hazy view of the fundus and retinal hemorrhage (Figure 1A1, 1B1, 1A2, 1B2). The previous hospital’s diagnosis was acute retinal necrosis. The patient was given intravenous and intravitreal injections of ganciclovir. Polymerase chain reaction (PCR) testing of the aqueous humor revealed positive cytomegalovirus (CMV)-DNA, while herpes simplex virus (HSV)-DNA, varicella zoster virus (VZV)-DNA, and Epstein-Barr virus (EB)-DNA were all negative. The ratio of aqueous IL-10/IL-6 was less than 1. According to these results, the hospital changed the patient’s diagnosis to CMV retinitis, and two other consecutive intravitreal injections of ganciclovir were given. However,the patient’s BCVA decreased to hand movement (HM) with severe vitreous opacity, and ultrasonography revealed retinal detachment of the right eye (Figure 1A3, 1B3). Therefore, the patient was referred to our hospital for further treatment.
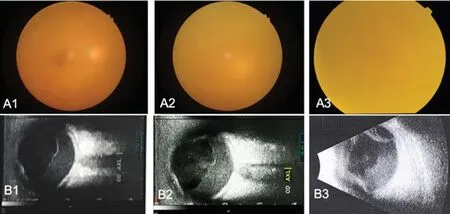
Figure 1 Fundus photo (A1) and B-scan ultrasound (B1) of the right eye at the early onset of the disease revealed uniform infiltration of the vitreous and a hazy view of the fundus. After the first intravitreous injection of ganciclovir, the fundus photo (A2)and B-scan ultrasound (B2) showed an aggravation of the vitreous opacity. After three intravitreous injections of ganciclovir, the fundus photo (A3) and B-scan ultrasound (B3) showed further aggravation of vitritis and retinal detachment.
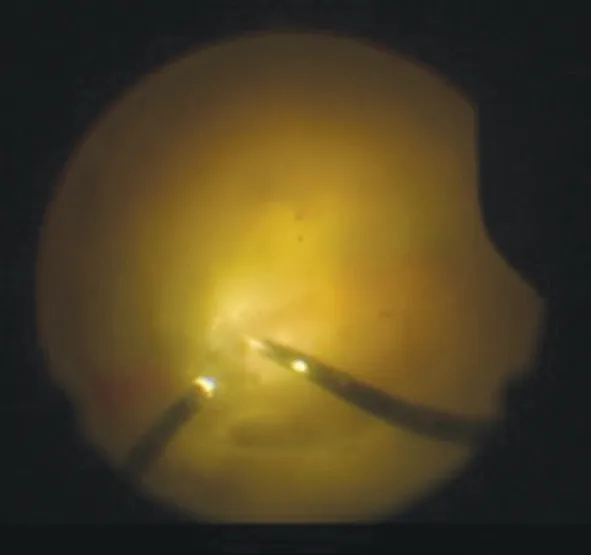
Figure 2 Fundus photo during vitrectomy of the right eye showed yellow-white purulent material in the vitreous cavity and on the surface of the retina.
The patient had tuberculosis 30 years ago and recovered after two years of treatment. She denies any other history of systemic disease. She was admitted to our hospital after respiratory consultation and exclusion of active tuberculosis.The patient underwent right eye diagnostic vitrectomy under local anesthesia. Vitreous smear samples were sent to the microbiology laboratory to look for bacteria, spores, fungal filaments and acid-fast bacilli. Bacterial culture and drug sensitivity tests as well as fungal cultures were also carried out.During the operation, a large amount of cloudy yellow-white purulent matter was observed in the vitreous cavity and in front of the retinal surface on the posterior pole (Figure 2). After clearing the cloudy vitreous, extensive retinal detachment,gray-white retinal edema and narrow retinal vessels were revealed. The results of the vitreous smear showed Gramnegative bacilli with a large number of white blood cells(Figure 3). The acid-fast staining and fungal smear results were all negative. According to these results, a diagnosis of bacterial ophthalmitis was made. A total of 400 μm/mL ceftazidime was immediately added to the vitreous infusion, and a thorough vitrectomy, lensectomy, electrocoagulation retinal incision,intraocular laser photocoagulation and silicon oil implant were carried out. The patient also received an intravenous infusion of ceftazidime twice daily after the operation. At this time, the patient recalled that she had experienced cold symptoms 2wk before the onset of the right eye symptoms but denied fever or any special treatment for those symptoms. However, the results of the bacterial culture were negative. Further diagnosis of the vitreous fluid by metagenomic next-generation sequencing(mNGS) was made. The DNA from the vitreous fluid was extracted with the TIANamp Micro DNA kit (TIANGEN,China). Then, the extracted DNA was sonicated to generate 150-200 bp fragments. After that, the DNA libraries were built based on the acquired DNA fragments according to the standard protocol of the BGISEQ-50 sequencing platform.Finally, the quantified libraries were sequenced with the BGISEQ-50 platform, and the sequencing data were analyzed with a Bioinformatics pipeline developed by Beijing Genomics Institute (BGI)[7]. We found that the total number of microbial reads was 268; however,Burkholderia cepacianaccounted for the highest number of microbial reads of 49 (18.28% of the total microbial reads). Therefore, we determinedBurkholderiainfection based on the mNGS results described above, and we speculated that thisBurkholderiahad ceftazidime sensitivity according to the laboratory analysis and clinical experience.Four months after the surgery, the BCVA in the right eye improved to 0.3; there was no anterior segment inflammation in the anterior segment; and the vitreous cavity was filled with silicone oil with good retinal reposition (Figure 4). The silicone oil was removed 9mo later, and the BCVA improved to 0.5 with retinal attachment.
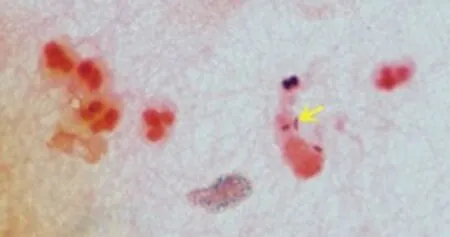
Figure 3 Vitreous smear showed Gram-negative bacilli (yellow arrow) and numerous white blood cells.
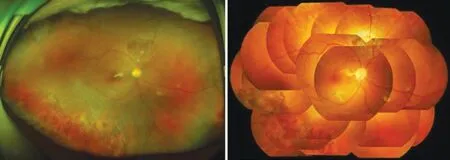
Figure 4 Fundus montage photo and fundus photo with an ultrawide view of the right eye showed good retinal reposition four months after vitrectomy.
DISCUSSION
Endophthalmitis caused byBurkholderiais rare. It has been reported to occur after ocular surgery, including cataract surgery and vitrectomy, resulting in the outbreaks of postoperative endophthalmitis due to the contamination of ophthalmic solutions, such as intraoperative topical anesthetic eyedrops and intraoperative trypan blue[5-6]. Okonkwoet al[8]reported 5 cases of endophthalmitis after vitrectomy with silicone oil filling, 3 of which demonstrated isolatedBurkholderiain the silicone oil. Silicone oil is believed to have some antimicrobial activity against common infectious endophthalmitis, so silica-related endophthalmitis is very rare, but suggested that silicone oil has no antibacterial effect againstBurkholderia. Saffra and Moriarty[9]reported a case of patient who presented 15d after injection of ranibizumab for neovascular age-related macular degeneration with culturepositiveBurkholderia cepaciaendophthalmitis. Irvineet al[10]reported one case ofBurkholderia cepaciaendophthalmitis following trauma. There is only one case report of endogenous endophthalmitis caused byBurkholderia pseudomalleiin a patient with melioidosis[11]. Unfortunately, we could not identify the source of infection in our case.
The following causes ofBurkholderiainfection in this patient were considered. First, the patient had a history of tuberculosis and had cold symptoms two weeks before symptom onset. Although she denied any other systemic history of immunodeficiency, the possibility ofBurkholderiaendophthalmitis caused by endogenous infection could not be completely excluded. Second, the patient was diagnosed with acute retinal necrosis and CMV retinitis in another hospital at the beginning of disease onset, but the condition worsened after three vitreous injections. Considering previous reports onBurkholderiaendophthalmitis, the possibility of infection after intravitreous injection should be considered. According to the quality control standard of intravitreous injection in China,it is recommended to use 5% povidone iodine to immerse the conjunctival sac for disinfection before injection in order to prevent infection[12]. However, studies have found thatBurkholderiacan grow in povidone iodine[13]; hence, povidone iodine immersion is ineffective for preventingBurkholderiainfection. In addition,Burkholderiacan be grown in a variety of media, such as conventional blood agar. However, the growth ofBurkholderiais so slow that the colony is usually very small.If not familiar withBurkholderiabacteria, the laboratory staffmight miss the identification in bacterial culture.
Vision loss and red eye pain are the two main clinical symptoms of bacterial endophthalmitis, but 25% of the reported cases indicate no significant eye pain[14]. Previous studies have reported that the clinical manifestations ofBurkholderiaendophthalmitis are decreased vision with no obvious ocular pain and mild anterior segment inflammation,occasionally with hypopyon, vitritis, and mild retinal dissolution[15]. In the early stage of the disease, our patient presented with decreased vision and redness in the eyes without any eye pain, accompanied by severe anterior segment inflammation and obvious vitreous inflammatory opacity.Therefore, the patient was misdiagnosed with acute retinal necrosis and CMV retinitis. The diagnostic criteria for acute retinal necrosis include sharp loss of vision, corneal edema,mutton-fat keratic precipitates, anterior chamber inflammation without posterior adhesion, vitreous inflammation, retinal vascular arteriolitis, and yellow-white necrotic lesions of the peripheral retina. CMV retinitis is often observed in immunecompromised patients with opportunistic infections. The clinical characteristic is that the yellow-white retinal necrosis lesion in the posterior pole along vessels is accompanied by prominent hemorrhage, presenting as “cottage cheese with ketchup”, with slight or no anterior segment inflammation or vitritis. However, the right eye of our patient had keratic precipitates with posterior iris adhesions and severe vitritis with no view of the fundus. Ultrasonography showed dense and uniform vitreous opacity with retinal detachment. No obvious retinal necrosis was observed in the fundus during or after vitrectomy, which does not conform with the findings of acute retinal necrosis or CMV retinitis.
Burkholderiaendophthalmitis can be treated with local,systemic, and intraocular sensitive antibiotics and vitrectomy with silicone oil tamponade[5-6], but this treatment is usually associated with poor visual outcomes, as reported in a previous study[6].Burkholderia cepaciaproduces lipopolysaccharide and β-lactamase, making it intrinsinsically resistant to aminoglycosides, and first- and second-generation cephalosporins[16]. Therefore, persistence of infection is common withBurkholderia cepacia, as reported in a case of recurrent endophthalmitis[17]. Our patient had good results,possibly due to the timely treatment, where ceftazidime was added into the vitreous infusion immediately according to the bacterial smear results and was combined with systemic ceftazidime treatment after the surgery.
In conclusion, a detailed medical history and first-hand clinical information are the basis of diagnosis. It is crucial for doctors to master the ocular manifestations of bacterial endophthalmitis, including the clinical symptoms and signs as well as anterior segment, vitreous, fundus and ultrasound features. Searching for the etiology is crucial in endophthalmitis, and diagnostic vitrectomy can determine both treatment and diagnosis.Burkholderiaendophthalmitis is rare and may have good prognostic results if treated timely and effectively.
ACKNOWLEDGEMENTS
Authors’ contributions:Chen H, Zhang JJ, and Ye JJ contributed to patient care, literature search, data collection,and writing of the report. Zhang JJ and Xu YC contributed to data analysis and data interpretation. All authors have read and approved the final manuscript.
Conflicts of Interest:Chen H,None;Zhang JJ,None;Xu YC,None;Ye JJ,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Protective effects of upregulated HO-1 gene against the apoptosis of human retinal pigment epithelial cells in vitro
- Spontaneous resolution of traumatic cataract after removal of a ferrous intravitreal foreign body using external magnetic extraction through a pars plana incision
- Glaucoma secondary to trabecular meshwork precipitates: a case report of Grant’s syndrome
- Histological observation in pachyvessels in a patient with choroidal melanoma
- Clinical characteristics and prognostic factors for visual outcome in 669 patients with intraocular foreign bodies
