Technical aspects in pancreaticoduodenectomy and therapeutic strategies for pancreatic cancer: History, current status, and future perspectives
Tomohide Hori , , Diki Ysukw
a Department of Surgery, Shiga General Hospital, Moriyama 524-8524, Japan
b Department of Surgery, Shiga University of Medical Science, Otsu 520-2192, Japan
The incidence of pancreatic cancer (PC) has increased, and invasive ductal adenocarcinoma is the most common among PC patients [1] . Even in patients who receive radical treatments, namely chemotherapy and surgery, the five-year survival is only 2%-9% [1] .Currently, many physicians recognize that further developments in multidisciplinary therapy are crucial to overcome PC [1] .
Pancreaticoduodenectomy is the primary therapy for malignancies in duodenal ampulla of Vater, extrahepatic biliary duct, pancreatic head and the uncinate process. In particular, this surgery plays an important role in multidisciplinary therapy for PC, although intractable complications and refractory symptoms may occur postoperatively, and a postoperative mortality of < 10% has been documented [2] . In this paper, we present the history, current status, and future perspectives of the technical aspects of pancreaticoduodenectomy and the therapeutic strategies for PC.
Pancreaticoduodenectomy has a fascinating history. In 1989,Alessandro Codivilla (1861-1912) first attempted to perform pancreaticoduodenectomy. Thereafter in 1912, Walther Kausch (1867-1928) realized successful pancreaticoduodenectomy. Allen Oldfather Whipple (1881-1963) verified the safety and feasibility of classic pancreaticoduodenectomy in 1935, and technical cues and functional recovery were documented. In 1944, Kenneth Watson initially described pylorus-preserving pancreaticoduodenectomy. Clinical utility was subsequently reported. Joseph G. Fortner introduced an extended pancreaticoduodenectomy (“regional pancreatectomy”) for better surgical curability in 1973. From the 1990s, to reduce delayed gastric emptying, subtotal stomach-preserving pancreaticoduodenectomy was introduced in Japan.
Inherent reconstructions are needed during pancreaticoduodenectomy. All pancreaticoduodenectomies require three reconstructions: digestive tract, pancreatic duct and biliary tree. Whipple, Charles G. Child III (1959-1978) and Hajime Imanaga (1902-1997) have proposed reconstructive procedures, and thereafter,their techniques have undergone modifications. Simple pancreaticoduodenectomies which omit extended dissections of lymphatic node (LN) and neuroplexus and/or intentional resections of regional vessel and nearby organ are clearly safe and feasible, and are widely used, mainly for benign diseases. However, pancreatic surgeons have questioned whether simple pancreaticoduodenectomy for benign diseases carries a higher risk. The answer is “No”;surgical techniques during pancreaticoduodenectomy are discussed in detail, and currently well-consolidated. Duct-to-mucosa pancreaticojejunostomy was first introduced by Richard Lynn Varco(1912-2004) in 1945, and anastomoses using the pancreatic duct,parenchyma, jejunal mucosa and/or seromuscular layer are currently well-established (e.g., the Kakita interrupted suture and modified Blumgart mattress suture).
Mortality and morbidity after pancreaticoduodenectomy are still critical issues. The mortality after pancreaticoduodenectomy has currently fallen to < 10% [2] . In fact, a facility’s ability [3] and individual surgeon’s skill [4] easily affect outcomes after pancreaticoduodenectomy. Advanced PCs may force pancreatic surgeons to extendedly resect regional vessel and nearby organ and to intentionally dissect neuroplexus and LN. However, these procedures are inherently invasive, and therefore, complications such as gastric or anastomotic ulceration, delayed gastric emptying, anastomotic failure, repeated cholangitis, abscess formation, pseudoaneurysm rupture, fatal hemorrhage and refractory pancreatic leakage may easily occur after pancreaticoduodenectomy. Especially, complications related with pancreatic juice are intractable and refractory. Postoperative pancreatic leakage generally results in pancreatic fistula.Regarding postoperative state of pancreaticoduodenectomy, refractory complication accompanied with intractable symptom and lifethreatening condition (e.g., septic state and massive hemorrhage)are serious nightmare for pancreatic surgeons. Pseudoaneurysm rupture causes sudden-onset, massive, and active hemorrhage, and this complication results in fatal outcomes. Leaving approximately 1 cm of the stump of the gastroduodenal artery, spreading an omental flap, and winding the round ligament of the liver spirally around the hepatic artery have been suggested to minimize direct contact of pancreatic juice with adjacent vessels, to prevent this fatal complication. Local continuous lavage has also attracted attention to minimize pancreatic juice-related complications.
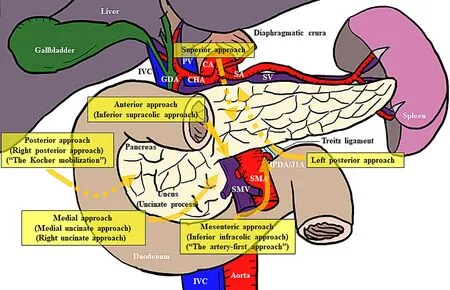
Fig. 1. Important approaches and technical aspects in pancreaticoduodenectomy.Posterior (right posterior), anterior (inferior supracolic), medial (medial uncinate or right uncinate), superior, mesenteric (inferior infracolic) and left posterior approaches are technical cues for pancreaticoduodenectomy. CA: celiac artery; CHA: common hepatic artery; GDA: gastroduodenal artery; IPDA: inferior pancreaticoduodenal artery; IVC:inferior vena cava; J1A: the first jejunal artery; PV: portal vein; SA: splenic artery; SMA: superior mesenteric artery; SMV: superior mesenteric vein; SV: splenic vein.
Important surgical approaches have been indicated for pancreaticoduodenectomy. The important approaches during pancreaticoduodenectomy are summarized in Fig. 1 ; however, all approaches should be performed during pancreaticoduodenectomy. The landmark of the posterior approach is the left adrenal vein flowing into the left renal vein; however, in 1902, Kocher originally mobilized the duodenum only to explore the inferior vena cava and pancreatic head (“the Kocher mobilization”). Among the key techniques during the superior and left posterior approaches, both sides of the celiac artery (CA) should be skeletonized sufficiently.Nakao and Takagi first described the mesenteric approach in 1993 [5] , and complete clearance around the superior mesenteric artery (SMA) by this approach might increase surgical curability for PC, leading to a decreased recurrence and improved survival. The phrase “artery-first approach” was first coined by Weitz et al. in 2010 [6] , and this term was adopted in 2012 [7] . This approach has advantages regarding surgical curability, clearance around the SMA,and less intraoperative blood loss [ 5 , 8 ]. The artery-first approach is mainly related to locally advanced PC.
Extended procedures have been established for PC. Graphical and surgical curability (i.e., R0 resection) is the primary goal in PC because even miniscule residual tumor is correlated with extremely poor outcomes. Extended resections of vessels [e.g., the superior mesenteric vein (SMV), portal vein (PV), SMA, and CA] and surrounding organs and intentional dissections of nerve plexuses and LNs may be indicated for PC patients, on a case-by-case basis.
The concept of a “mesopancreas” was suggested in 2007 [9] ,which was located in the retropancreatic area [10] . Connective tissue, loose areolar tissue, adipose tissue, nerve plexuses, lymphatic ducts, and capillary vessels extend from the pancreatic head, neck, and the uncinate process to the aortocaval groove [10] .The mesopancreas is continuous and connected to the paraaortic area, and the duodenum, pancreas and SMA form a complex of morphological, developmental, functional, and pathological structures [10] . However, the mesopancreas is a controversial structure and anatomically unconfirmed [11] . The mesopancreas is distinct from the mesorectum because a fascial envelope is never observed [11] ; therefore, the mesopancreas should be considered a surgical concept, rather than an anatomical structure.Beyond the “artery-first” concept in pancreaticoduodenectomy for PC, pancreatic surgeons currently focus on “mesopancreas-first”pancreaticoduodenectomy (e.g., the Cattell-Braasch maneuver). According to the concept of total mesorectal excision [9] , total mesopancreas excision, which constitutesenblocand systemic resection of the mesopancreas, has been proposed. Adham and Singhirunnusorn [12] first described total mesopancreas excision for pancreaticoduodenectomy, and since then, this excision during pancreaticoduodenectomy has been considered safe and feasible for PC [8]. Furthermore, total mesopancreas excision increases surgical curability and improves prognostic outcomes [ 8 , 12 ].
Intentional dissections of nerve plexuses and LNs may be indicated for PC patients [ 8 , 13-15 ], although the therapeutic benefit of these intentional dissections is controversial. Extended lymphadenectomy of paraaortic LNs may be indicated especially for PC located at the body or the uncinate process, because these PCs are close to paraaortic LNs [13-15] . Regarding intentional LN dissection, some pancreatic surgeons deny the effectiveness of this procedure, although others believe this procedure to be beneficial [13-15] . Regarding intentional dissection of nerve plexuses,this dissection during total mesopancreas excision was positively evaluated [ 8 , 12 ], although some surgeons denied its effectiveness around the SMA.
Locally advanced PC is a matter of debate. PC is associated with low resectability. To adequately deal with PCs, PCs are classified into resectable, borderline resectable (partially invaded into SMV, PV, SMA or CA) and unresectable (locally advanced and metastatic) [16] . Locally advanced PC remains a critical matter, and therapeutic strategies should be established in the near future.Chemotherapy or chemoradiotherapy is initially indicated for locally advanced PC, even though extended surgery is subsequently set. PC located at the uncinate process easily invades the SMV/PV and nerve plexuses around the SMA because of anatomical proximity, and the optimal therapeutic strategy may differ among various subgroups within the category of locally advanced PC. Venous invasion into the SMV and/or PV affects prognostic outcomes after pancreaticoduodenectomy, and arterial invasion into nerve plexuses around the SMA and/or CA may be comparable to venous invasion regarding pancreaticoduodenectomy efficacy and prognostic outcomes. Pancreaticoduodenectomy accompanied by resection of the PV and/or SMV and intentional dissection of nerve plexuses around the CA and SMA is safe and potentially beneficial for PC patients.
We should never forget future perspectives for PC. Neoadjuvant chemotherapy is currently induced even in patient with resectable PC. Neoadjuvant chemotherapy is also indicated for borderline resectable PC, because surgery alone shows insufficient outcome.Chemotherapy or chemoradiotherapy is induced for unresectable PC, although conversion surgery may be indicated after the initial therapy. In particular, therapeutic strategy for borderline resectable or locally advanced PC is a matter of debate between surgery,chemotherapy or chemoradiotherapy. Therapeutic strategy should be carefully decided on a case-by-case basis.
In cases of borderline resectable patients, upfront surgery alone is insufficient; therefore, neoadjuvant chemotherapy [e.g., gemcitabine + S1, gemcitabine + nab-paclitaxel and FOLFIRINOX (i.e.,irinotecan, fluorouracil, leucovorin and oxaliplatin)] is currently indicated for this population. Moreover, neoadjuvant chemotherapy is recommended even in cases of resectable PC, and adjuvant chemotherapy (e.g., FOLFIRINOX) is important, especially in cases of borderline resectable patients. Pancreaticoduodenectomy as conversion surgery may be indicated in cases of initially unresectable PC. The median survival after conversion surgery is approximately 3 years; however, the reported median survival is 2.3 years in patients with peritoneal dissemination. These prognostic outcomes after conversion surgery appear to be acceptable. Conversion surgery should be indicated without distinction on the basis of locally advanced tumors or distant metastases because there are no differences in survival between these populations.
Circulating tumor cells correlate with prognostic outcomes in PC patients, and multidisciplinary therapy is considered important for successful treatment [1] . Although a facility’s ability [3] and individual surgeon’s skill [4] easily effect outcomes after pancreaticoduodenectomy, this surgery is an important key for successful multidisciplinary therapy for PC. Regarding advanced surgery, robotic pancreaticoduodenectomy may spread worldwide in the near future.
The radical resection in pancreaticoduodenectomy is increasing thanks to the technical improvements, and the role of surgery in the multidisciplinary approach of locally advanced PC has to be assessed by further series.
In conclusion, pancreatic surgeons have a large frontier. The question can be asked, “Where should pancreatic surgeons head in the next decade?” We consider it important to focus on improving the prognostic outcomes of PC with multidisciplinary therapy,including pancreaticoduodenectomy.
Acknowledgments
None.
CRediT authorship contribution statement
Tomohide Hori: Conceptualization, Data curation, Formal analysis, Investigation, Supervision, Validation, Writing - original draft,Writing - review & editing. Daiki Yasukawa: Data curation, Formal analysis, Investigation, Validation, Visualization, Writing - review &editing.
Funding
None.
Ethical approval
This study was approved by the Institutional Review Board of Nagai General Hospital, Tsu, Japan.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2022年6期
Hepatobiliary & Pancreatic Diseases International2022年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- YAP activates pancreatic stellate cells and enhances pancreatic fibrosi s
- Combined analysis of imaging tumor capsule with imaging tumor size guides the width of resection margin for solitary hepatocellular carcinoma
- Prediction of early recurrence of hepatocellular carcinoma after liver transplantation based on computed tomography radiomics nomogram
- Complications of modern pancreaticoduodenectomy: A systematic review and meta-analysis
- Contrast-enhanced ultrasound predicts microvascular invasion in patients with hepatocellular carcinoma
- Safety and immunogenicity of COVID-19 vaccination among liver transplant recipients in China
