Role of the ultra-wide-field imaging system in the diagnosis of pigmented paravenous chorioretinal atrophy
Ya-Ling Liu, Ya-Rou Hu,2, Miao-Hong Chen, Zhen Yu, Guo-Ming Zhang,2
1Shenzhen Eye Hospital, Jinan University, Shenzhen Eye Institute, Shenzhen 518040, Guangdong Province, China
2Department of ophthalmology, the Second Clinical Medical College of Jinan University, Guangzhou 510632, Guangdong Province, China
Dear Editor,
P igmented paravenous chorioretinal atrophy (PPCRA),which was first described by Hewiston-Brown in 1937, is a rare pigmentary retinopathy affecting the retina and choroid;most patients mainly manifest symmetrical retinal choroid in both eyes, except for a small number of patients with monocular manifestations[1]. The condition is characterized by atrophy and pigmentation along the great retinal vein and its branches. The cause of PPCRA is not yet clear; however, the suspected pathogenic factors include inflammation, infection,and genetics[1]. Ultra-wide-field (UWF) imaging is a promising tool for the diagnosis and treatment of peripheral retinal and choroidal diseases. Ordinary UWF systems still have problems such as unclear peripheral images, eyelash artifacts, and weak penetrating ability. It is difficult to diagnose small retinal tears and retinal detachments in the eye. The UWF imaging(CLARUS 500?, Carl Zeiss Meditec AG, Jena, Germany),which is a UWF retinal imaging system designed to cover up to 133° of the retina in a single image, features partially confocal optics and true color imaging, which are not available in the Optos[2]. Herein, we described for the first time the use of the UWF imaging to image the fundus of patients and their immediate family members because the diagnosis of PPCRA is based on characteristic fundus manifestations and the UWF imaging can provide clear and broad fundus images. With the help of genetic testing, we suspected that there is no related genetic factor between the patient and her immediate family.
We present two patients. One of these is a 4-year-old female child who was found to have poor vision in her right eye during the kindergarten physical examination. She was born at full term, and her parents denied any family history of hereditary eye diseases, trauma, and infectious diseases. The naked vision of both eyes is finger counting (FC)/40 cm in the right eye and 20/40 in the left eye. Her best-corrected visual acuity was FC/40 cm in the right eye (+3.50/1.50×15°) and 20/25 in the left eye (+4.50/1.00×5°). The examination of the anterior segment of both eyes showed no abnormalities. The results of Zeiss IOLMaster-700 showed that both eyes had a slightly shorter axial length and a larger mean radius of the curvature of the cornea (8.25 mm). The UWF imaging showed retinal choroidal atrophy and pigment accumulation near the veins of both eyes, with the right eye involving the macular area (Figure 1A). The affected area showed high fluorescence with clear boundaries (Figure 1B). Optical coherence tomography-enhanced depth imaging (OCT-EDI) showed that the inner core of the retina was disordered with mild choroidal atrophy in both eyes (Figure 1C). A diagnosis of bilateral PPCRA was made, and the patient was advised routine followup every three months.
Another patient is the 3-year-old brother of the patient who had a history of intermittent esotropia with corneal reflection about +35°. His parents denied any family history of hereditary eye diseases, trauma, and infectious diseases. Due to the poor coordination of the child, the results of specific vision were not clear. The optometry result of ciliary muscle palsy was+2.50/1.00×100° for the right eye and +6.50 for the left eye.The results of IOLMaster-700 showed that the axial length of the patient’s eyes was slightly shorter. The UWF imaging showed retinal choroidal atrophy and pigment accumulation besides veins in both eyes and no accumulation of macular area in both eyes (Figure 2A). The affected area showed high fluorescence with clear boundaries (Figure 2B). OCT-EDI showed the disappearance of the fovea in both eyes (Figure 2C). A diagnosis of bilateral PPCRA was made, and the patient was advised routine follow-up every three months.
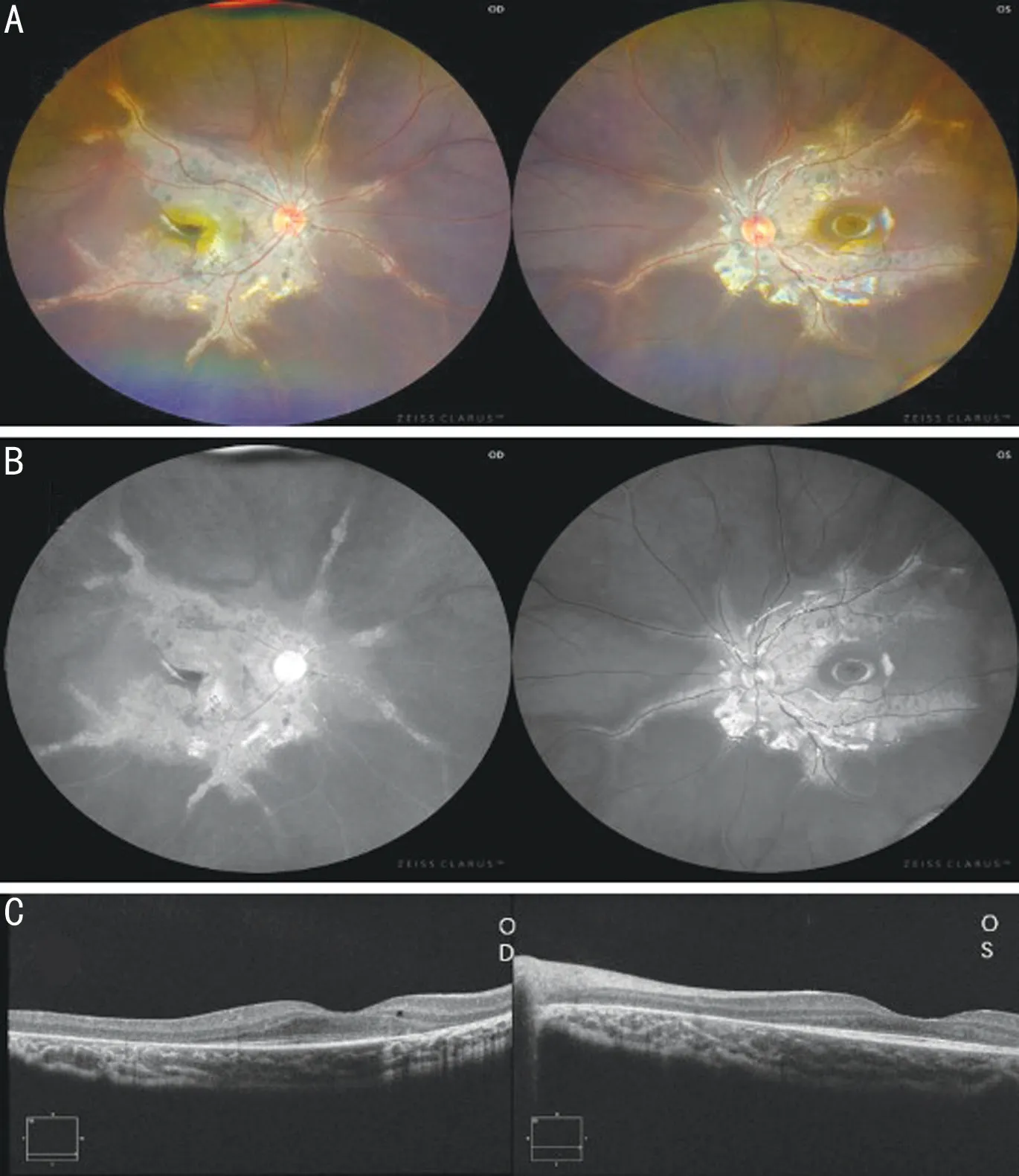
Figure 1 The UWF fundus photographs and OCT-EDI of case 1 A: The UWF fundus photographs of case 1 with retinal choroidal atrophy and pigment accumulation near the veins of both eyes with the right eye involving the macular area; B: FAF images show high fluorescence with clear boundaries; C: OCT-EDI shows that the inner core of the retina is disordered with mild choroidal atrophy in both eyes. UWF: Ultra-wide-field; FAF: Fundus auto-fluorescence; OCTEDI: Optical coherence tomography-enhanced depth imaging.
The UWF imaging results showed that both cases had similar characteristic fundus manifestations. Combined with the patients’ medical history and related examination results,the diagnosis can be confirmed. Due to the poor cooperation ability of the patients and family members, fundus fluorescein angiography (FFA) and related retinal electrophysiological examinations were not done. Taking into account the genetic factors reported by McKayet al[3]and others for PPCRA, the father and mother of both patients also underwent examination using the UWF imaging and routine eye examinations. All four of them were tested for related genes. The UWF imaging showed that the mother’s fundus presented binocular retinitis pigmentosa (RP), and she was diagnosed with RP (Figures 2D and 2E). The patients’ father had no abnormalities in the fundus (Figure 2F). The genetic test result showed that the 4-year-old female patient had MMP19 mutation, her father and younger brother were heterozygous for PRPF4, and her mother had no genetic abnormalities.
The study was conducted in accordance with the principles of the Declaration of Helsinki. The informed consent was obtained from the patients’ guardians.
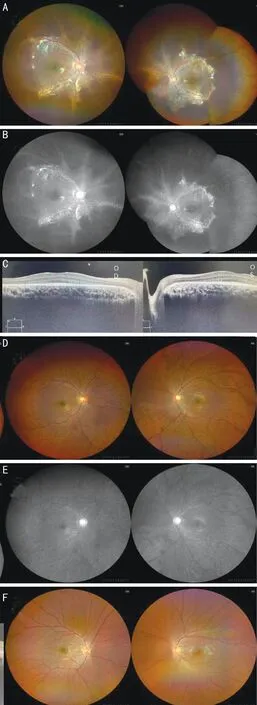
Figure 2 The UWF fundus photographs and OCT-EDI of case 2, case 1’s mother and case 1’s father A: The UWF fundus photographs of case 2 with retinal choroidal atrophy and pigment accumulation near the veins of both eyes with the right eye involving the macular area; B: FAF images show high fluorescence with clear boundaries;C: OCT-EDI shows the disappearance of the fovea in both eyes; D:The UWF imaging shows osteocyte-like pigment of the fundus of the mother, involving the posterior pole and peripheral retina of both eyes except the macula; E: FAF images showing hypo-fluorescence in pigmented areas; F: The UWF imaging of the father’s roughly normal fundus. UWF: Ultra-wide-field; FAF: Fundus auto-fluorescence;OCT-EDI: Optical coherence tomography-enhanced depth imaging.
We found that the fundus images of the 4-year-old female patient and her brother showed significant pigment accumulation not only along the retinal vein, but also extending to the surrounding area, forming a butterfly-like lesion centered on the optic papilla. In particular, the lesion in the patient’s right eye involved the macular area, which may also be the cause of the patient’s low vision. This is inconsistent with reports in most articles that the disease rarely affects the macular area and that children are asymptomatic[1,4]. Kumaret al[5]described that the onset of PPCRA starts from the site far away from the optic nipple, but we found that most of the images in the article involved the optic nipple, including the two patients reported in the present article. The possible reason is that the patients reported in Kumaret al’s[5]article are all advanced patients.Considering the age and clinical manifestations of the two patients in the present article, another possible reason is that the onset of some patients starts from the optic papilla, or the diseased area of the patient has been consistent.
We also found a large amount of pigmentation in the fundus of the patients’ mother, except for the optic papilla and macular area. However, unlike the fundus auto-fluorescence (FAF)images of both patients, the mother’s FAF images showed low fluorescence, suggesting that the retinal pigment epithelium of the mother’s eyes may be in a state of atrophy. This kind of UWF imaging can make patients comfortable and reduce the rate of missed diagnosis and misdiagnosis, thereby reducing the economic burden on patients.
To further clarify whether the patients have genetic factors,genetic testing was performed on the patients and their immediate family members. The genetic test results suggested no related genetic factors between the patients and their immediate family members, which is different from theCRB1gene mutation site reported in a previous study[3]. This may be a new variant site, and it may also be one of the reasons why the etiology of PPCRA remains unclear. Unfortunately, due to the small size of the genetic testing family, we could not determine the genetic pattern. PPRCA has many similarities to RP in appearance. These two diseases may be essentially one type of disease. The reports[5-6]also fits this hypothesis.However, Nobel and Carr[7]suspected that the PPCRA of 23 patients was affected by acquired factors and had nothing to do with heredity, which also increased the need for PPCRA gene research.
We described for the first time the broad and clear fundus features of the UWF imaging system for PPCRA, which provides very strong support for the diagnosis of PPCRA.Through genetic testing, we suspected that part of the incidence of PPCRA is not related to heredity. As a non-invasive examination, the UWF imaging system helps to understand the pathogenesis and progress of PPCRA.
ACKNOWLEDGEMENTS
Foundations:Supported by Shenzhen-Hong Kong Cofunded Projects (Category A) (No.SGDX20190920110403741);Guangdong Basic and Applied Basic Research Foundation(No.2022A1515012326); Shenzhen Key Medical Discipline Construction Fund (No.SZXK038); Shenzhen Fund for Guangdong Provincial High level Clinical Key Specialties(No.SZGSP014); Shenzhen Science and Technology Program(No.JSGG20201102174200001).
Conflicts of Interest: Liu YL,None;Hu YR,None;Chen MH,None;Yu Z,None;Zhang GM,None.
 International Journal of Ophthalmology2022年11期
International Journal of Ophthalmology2022年11期
- International Journal of Ophthalmology的其它文章
- Paracentral acute middle maculopathy after diagnostic cerebral angiography in a patient with a contralateral carotid-cavernous fistula
- Optical coherent tomography angiography observation of macular subinternal limiting membrane hemorrhage in CO poisoning: a case report
- Choroidal folds associated with carotid cavernous fistula:a case report
- A rare combination of late-onset post-LASlK keratectasia after early-onset central toxic keratopathy
- Gastrointestinal microbiome and primary Sj?gren’s syndrome: a review of the literature and conclusions
- lnsights on the possibility of SARS-CoV-2 transmission through the eyes
