A rare combination of late-onset post-LASlK keratectasia after early-onset central toxic keratopathy
Mehrdad Mohammadpour, Masoud Khorrami-Nejad, Mohsen Heirani, Joseph Oleribe
1Translational Ophthalmology Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran 1416753955, Iran
2Department of Optometry, Imo State University, Owerri, Imo 2000, Nigeria
Dear Editor,
We have presented the clinical findings of a case with bilateral early-onset central toxic keratopathy (CTK)followed by bilateral late-onset post-LASIK keratectasia. Laserin situkeratomileusis (LASIK) is a safe procedure to treat a broad spectrum of refractive errors; however, unexpected and rarely encountered post-LASIK complications could be a challenge for patient and surgeon. Post-LASIK keratectasia is a significant consequence of the LASIK operation that may appear anywhere from one week to many years after the procedure[1]. Although the exact incidence rate of post-LASIK keratectasia remains debatable, it was estimated to be from 0.04 to 0.6%[1]. Post-LASIK keratectasia causes progressive corneal thinning, central/paracentral corneal steepening,irregular astigmatism, and reduced the best distance corrected and uncorrected visual acuity (CDVA and UDVA). CTK,another rare complication of this refractive procedure, is an acute and non-inflammatory central corneal opacity with following typical characteristics: anterior to mid-stromal opacification, marked corneal flattening, and significant hyperopic shift[2]. This complication has a documented incidence rate of 0.016 percent[2]and occurs mostly in the initial days after refractive surgery[3]. Although the fundamental cause of CTK is uncertain, intraoperative corneal toxicity from several sources has been shown to be influential[2-3]. Since CTK is non-inflammatory and self-limiting, no particular treatment intervention is required. Prior to this, no case of bilateral keratectasia preceded by CTK after LASIK refractive surgery, has been reported. In this report, the clinical findings of a patient with bilateral early-onset CTK followed by bilateral late-onset post-LASIK keratectasia are presented. No identifiable health information was included.
A 44-year-old male presented to the hospital in April 2002,seeking laser refractive surgery to treat the myopic astigmatism,having manifest refraction (MRX) of -6.25/-1.00×5 in the right eye (RE) and -5.75/-2.00×165 in the left eye (LE). The corneal topography data with Placido-disc topography (CSO topographer, Costruzione Strumenti Oftalmici) showed an average corneal power of 43.95 D in the RE, and 44.73 D in the LE (Figure 1). Central corneal thickness (CCT) in the right and the left eye was 545 and 552 microns, respectively. There were no systemic or ocular problems found, and the patient said that he had never undergone ophthalmic surgery before.
The patient underwent an uneventful microkeratome-assisted LASIK procedureviaNIDEK EC-5000 excimer laser (NIDEK Co. Ltd., Japan). The RE and LE had a corneal ablation depth of 104.6 and 110.5 microns, respectively. Following that, the RE’s residual stromal bed thickness was determined to be 280.4 microns and the LE’s to be 281.5 microns. The patient selection criteria were adequate since the minimal corneal thickness and minimum residual stromal bed cut-off values at the time of the LASIK procedure (2002) were 480 microns and 250 microns, respectively[4].
Ten days after surgery, he presented with the complaint of reduced vision in both eyes. His MRX revealed a significant compound hyperopic astigmatism shift: +8.25/-4.25×66 (CDVA=20/50)in the RE, and +6.75/-3.25×79 (CDVA=20/40) in the LE.Barely one month following this surgery, corneal topography recordings showed remarkable and abnormal central flattening(Figure 2A). The average corneal powers of the RE and the LE were 29.85 D and 32.27 D, respectively. The clinical observations revealed CTK. Moreover, in addition to the tapered administration of topical fluorometholone, the surgeon considered the ‘watchful waiting’ approach and prescribed topical lubricants to relieve eye irritation. Two months later,the patient presented with less abnormal corneal flattening,improved MRX and CDVA (MRX of +5.25/-1.50×91 and CDVA of 20/30 in the RE, as well as MRX of +6.25/-2.25×81 and CDVA of 20/30 in the LE). The corneal topography patterns and indices in both eyes were within normal limits after two years, compared to the corrected preoperative refraction (average corneal power rose to 35.44 D and 34.87 D,respectively; Figure 2B).
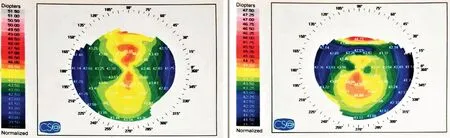
Figure 1 Preoperative corneal topography imaging of both eyes.
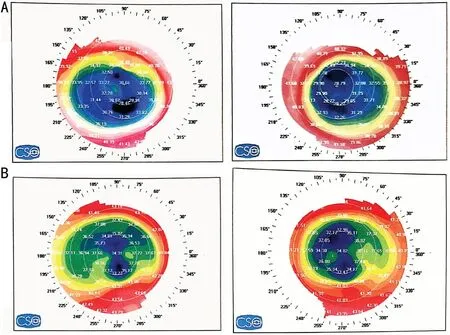
Figure 2 Abnormal central corneal flattening of the right and the left eye one month (A) and two years (B) after LASIK refractive surgery.
Four years after LASIK surgery, as shown in Figure 3A,early manifestations of keratectasia were observed on corneal topography patterns of both eyes which were recorded by scanning slit topography (Orbscan; Bausch & Lomb). Figure 3A shows the patterns or inferior steepening and posterior elevation. Because of suboptimal CDVA, the patient was fitted successfully with gas permeable (GP) contact lenses, and accordingly his CDVA increased to 20/20 in either eye. Figure 3B and 3C illustrate the refractive maps and Belin/Ambrósio enhanced ectasia display of the patient achieved by Pentacam HR (Oculus, Wetzlar, Germany) in 2018. The progressive post-LASIK keratectasia was revealed by higher values of inferior steepening and remarkable posterior and anterior elevations that were more severe in the RE. Regarding retinoscopic scissor reflexes, no clear refraction data were obtained. Also,the autorefractometry examination displayed variable and inconsistent data. His CDVA with subjective refraction was 20/40 in the RE and 20/30 in the LE. However, CDVA with GP lenses was 20/20 in either eye.
Figure 4 shows the anterior segment optical coherence tomography and pachymetry map of both eyes using Optovue(RTVue-100; Optovue Inc, Fremont, CA, USA) in late 2020. The epithelial map shows epithelium thickening and irregularities, especially in the LE. The epithelial changes are supportive data for the presence of post-LASIK karatectasia.
Figure 5 shows the clinical timeline of patient during 18-year follow-ups examinations.
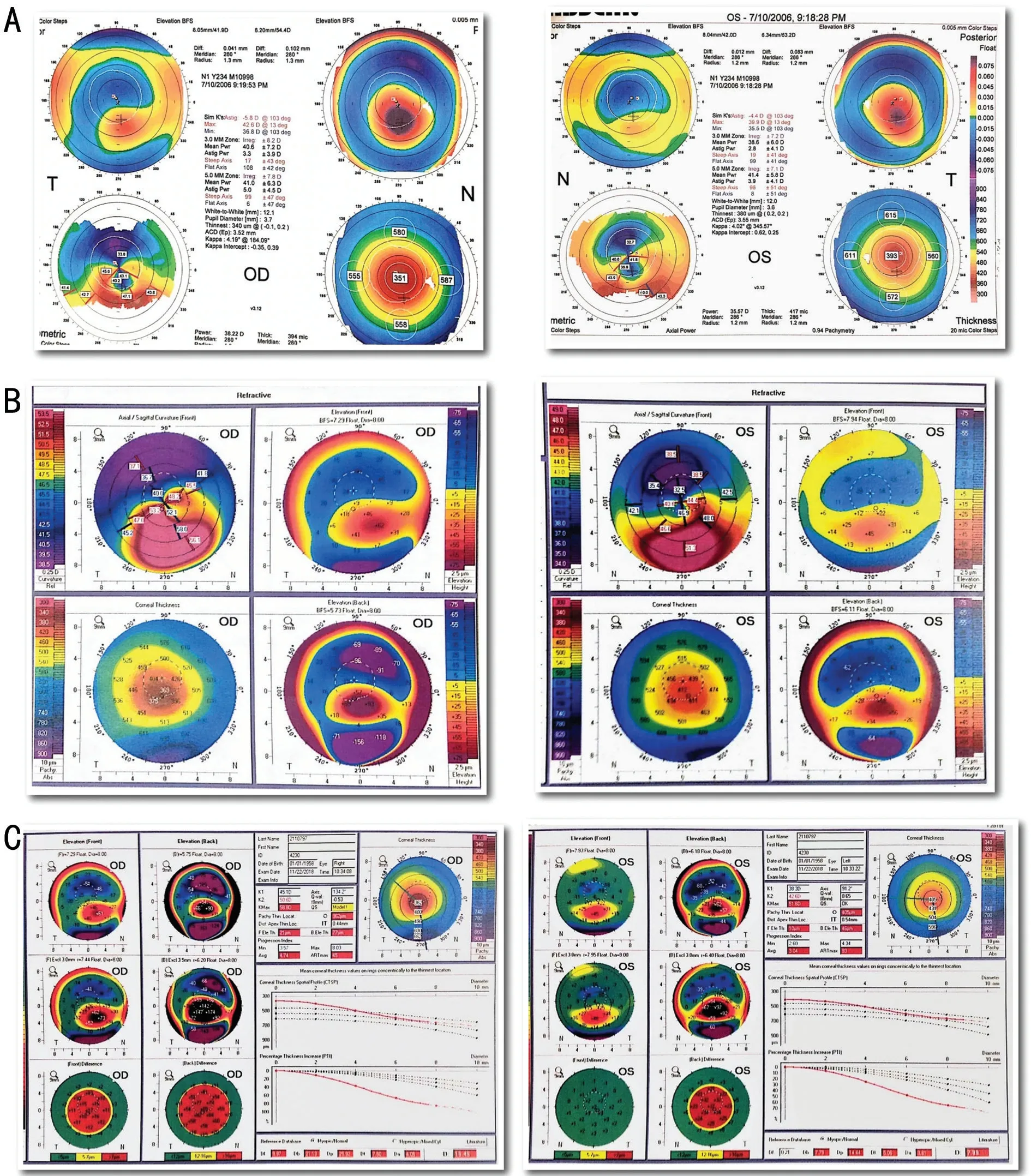
Figure 3 Post-LASIK keratectasia manifestations of the right eye and the left eye four years after LASIK surgery represented by four maps of Orbscan (A) and sixteen years after LASIK surgery represented with Pentacam HR refractive map (B), and Belin/Ambrósio display (C).

Figure 4 Eighteen years after LASIK refractive surgery, anterior segment optical coherence tomography and epithelial map of the right and left eyes.
This is the first case report of two unusual post-LASIK refractive surgical complications: early-onset CTK and lateonset post-LASIK keratectasia. The patient originally had a severe hyperopic refractive shift after LASIK surgery, as well as aberrant bilateral corneal flattening, which was symptomatic of CTK. Several years after completing CTK management, the patient presented with clinical manifestations of post-LASIK ectasia in both eyes, confirmed by corneal topography imaging.The patient was fitted with GP lenses and was suffering from long-term complications of LASIK procedure up to the final examination in November 2020.
Several hypotheses were assumed concerning the potential causes of CTK and post-LASIK keratectasia; however, the exact etiology remains a matter of debate[5].
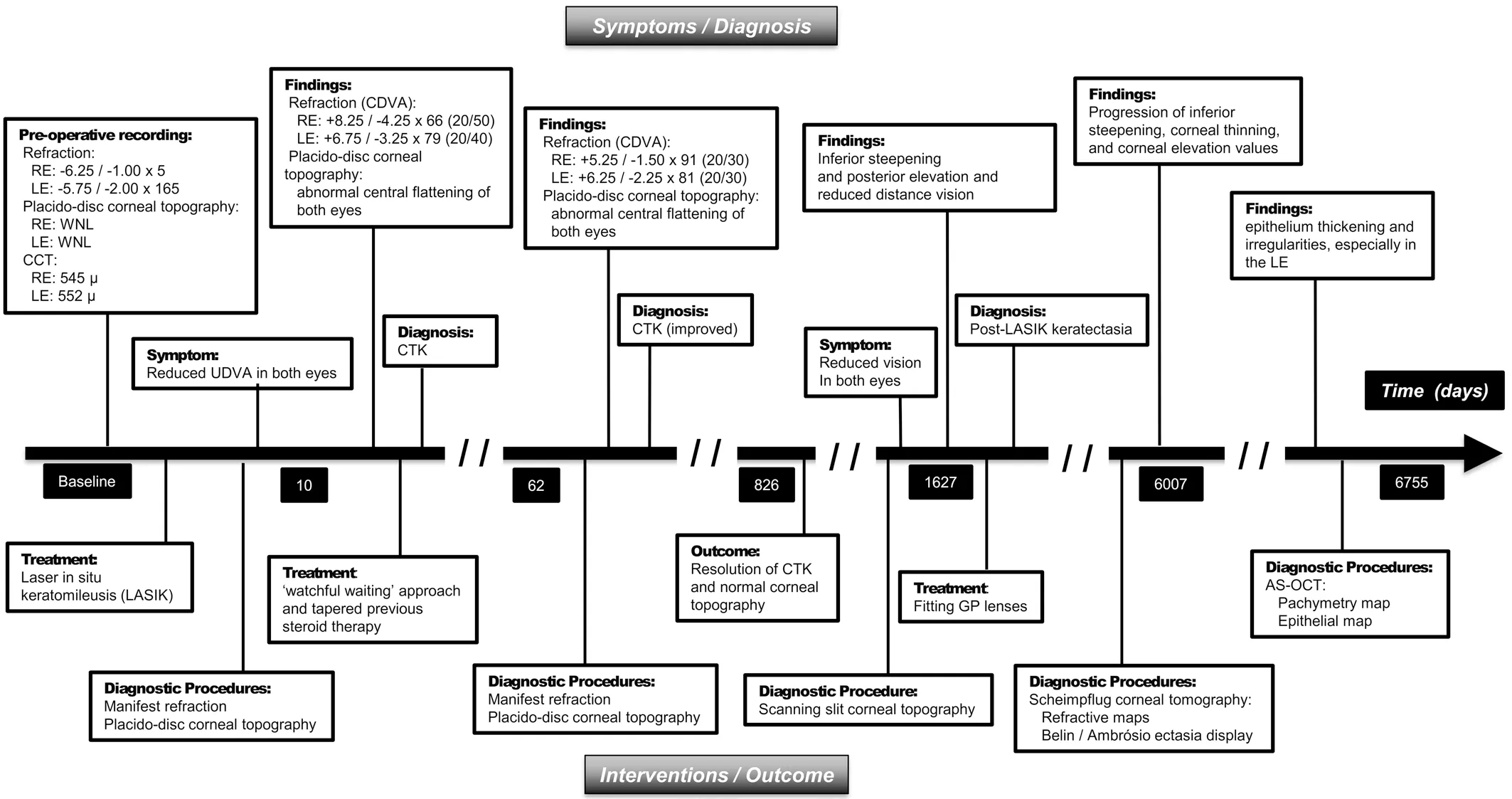
Figure 5 Clinical timeline of 44-year-old male diagnosed as early central toxic keratopathy and late post-LASIK keratectasia following LASIK surgery RE: Right eye; LE: Left eye; CTK: Central toxic keratopathy; CDVA: Corrected distance visual acuity; UDVA:Uncorrected distance visual acuity; GP: Gas permeable; AS-OCT: Anterior-segment optical coherence tomography.
CTK is a non-inflammatory corneal disease that usually appears during the first few days after laser refractive surgery and may last anywhere from 12 to 18mo[3]. Typical CTK symptoms were found in this instance, including aberrant corneal flattening, significant hyperopic shift, and reduced CDVA, which began after around ten days and resolved during the first two years after the LASIK procedure. Post-LASIK keratectasia is a severe complication and could be sight-threatening. It was found that this disorder might be associated with biomechanical weakening of the cornea and subsequent decrease of CDVA with conventional optical corrections[6]. Younger age, abnormal pre-surgery corneal topography, and a thin cornea are all potential risk factors for keratectasia[4,6]. Nonetheless, no specific preoperative risk factors were discovered to constitute an underlying mechanism for the development of postoperative keratectasia in this patient. Based on the preoperative measurements, the predicted residual stromal bed thickness was 276.25 microns and 275.75 microns for the right and left eyes, respectively. Currently,an updated metric determines the minimum residual stromal bed known as percent tissue altered (PTA)[7]. This index is calculated as (flap thickness + ablation depth)/preoperative CCT. The patients with PTA values of more than 40% are exposed to an increased risk of post-LASIK keratectasia even with typically normal preoperative corneal topography patterns. Considering the flap thickness of 160 microns, this patient had a PTA value of 48.5% in the RE and 49% in the LE at the time of LASIK surgery. However, it was indicated that the patients with higher PTA values do not necessarily develop post-LASIK keratectasia[7]. Based on calculated PTA index, preoperative data indicated that this patient might be relatively susceptible to postoperative keratectasia development.
After refractive surgery, post-LASIK keratectasia may appear as an early or late-onset complication. Around four years after the refractive operation, the first signs of post-LASIK keratectasia were seen. Keratectasia was present before the beginning of CTK in this patient. Although the specific cause of post-LASIK keratectasia is unknown, some researchers believe that failure in the postoperative corneal regeneration process may be a contributing factor[8]. According to this school of thought,keratocytes activation causes the intercellular release of degradative enzymes, thereby inducing corneal viscoelasticity weakening that may contribute to failure in the stromal remodeling process[8].
Sonmez and Maloney[2]reported that keratocyte apoptosis in CTK corneas might result in stromal tissue loss. This finding was corroborated in confocal microscopy studies which showedin vivostromal keratocyte changes in CTK corneas[9].Hurmericet al[10]found that corneal biomechanics was significantly correlated with stromal keratocyte density. They concluded that corneal viscoelastic properties were integral to the stromal matrix and cornea’s cellular structure. Dupps and Wilson[11], in a review study, concluded that changes in keratocytes and subsequent biomechanical failure could result in post-LASIK keratectasia. Furthermore, Liu and Manche[12]observed that AS-OCT imaging of CTK corneas revealed stromal bed thinning. Stromal thinning is an additional factor predisposing to weaken corneal biomechanics[1]. Mechanical microkeratome-assisted LASIK may be another risk factor in developing post-LASIK keratectasia and CTK[13]. As this case was operated using a mechanical microkeratome procedure, it could be assumed that the procedure would be another inciting factor in the occurrence of post-LASIK keratectasia and CTK.
Because of less accurate mechanical microkeratome flaps, the exact 160 microns’ flap thickness was not guaranteed, and it could be higher than the expected value. This issue could be an additional risk factor in developing post-LASIK keratectasia in this patient.
This study consequently posits that the LASIK procedure and subsequent occurrence of CTK may promote corneal biomechanical deterioration, which may lead to post-LASIK keratectasia. In other words, early postoperative CTK may contribute to the development of late-onset keratectasia.
ACKNOWLEDGEMENTS
Conflicts of Interest:Mohammadpour M,None;Khorrami-Nejad M,None;Heirani M,None;Oleribe J,None.
 International Journal of Ophthalmology2022年11期
International Journal of Ophthalmology2022年11期
- International Journal of Ophthalmology的其它文章
- Paracentral acute middle maculopathy after diagnostic cerebral angiography in a patient with a contralateral carotid-cavernous fistula
- Optical coherent tomography angiography observation of macular subinternal limiting membrane hemorrhage in CO poisoning: a case report
- Choroidal folds associated with carotid cavernous fistula:a case report
- Role of the ultra-wide-field imaging system in the diagnosis of pigmented paravenous chorioretinal atrophy
- Gastrointestinal microbiome and primary Sj?gren’s syndrome: a review of the literature and conclusions
- lnsights on the possibility of SARS-CoV-2 transmission through the eyes
