Glucagonoma syndrome with necrolytic migratory erythema as initial manifestation
Wei-Fng Zhu , Shu-Sen Zheng ,
a Department of Dermatology, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
b Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
TotheEditor:
Necrolytic migratory erythema (NME) is a group of cutaneous lesions characterized by periodic episodes of annular or figurative dark red plaques, which are typically accompanied by blisters,erosions, and crusting. It is often associated with glucagonoma.Glucagonoma is an extremely rare neuroendocrine tumor that arises from pancreatic isletαcells and manifests as elevated glucagon, with an incidence of about 1 in 20 million per year [ 1 , 2 ].Glucagonoma with NME is defined as glucagonoma syndrome (GS),and the presence of skin lesions helps in the timely diagnosis and treatment of pancreatic tumors [ 3 , 4 ]. Here we reported a case of GS with NME as initial manifestation aiming to improve our understanding of GS and achieve an early diagnosis.
A 54-year-old female patient had bilateral erythema, rhagades,and itching/pain on the dorsum of foot without any obvious cause 5 years ago, which was improved with topical erythromycin ointment but recurred after discontinuing the medication. These lesions gradually spread to the skin around the mouth, trunk, groin,buttocks and lower extremities, where the rashes fused together,along with the presence of blisters, erosions and crusting. Erosions were present at perioral area and tongue, causing difficulty in eating irritating food. No diarrhea was noted. The patient had sought treatment in other hospitals several times. The symptoms were alleviated after treatments with compound glycyrrhizin tablets or minocycline but recurred frequently. Two months ago, the rash worsened and was considered neutrophilic dermatosis in a local hospital. However, the rash was not alleviated after treatments, including an infusion of intravenous dexamethasone. The patient was then admitted to our hospital for further treatment.
Physical examination on admission showed that the skin of the trunk, lower legs, thighs, and buttocks had various sizes of edematous erythema, blisters, and pustules of various sizes, which had become ruptured and eroded; erosions on the tongue and around the mouth were irregular in shape, partly presenting as gyratus or migratory annular patches. Her lesion area/total body surface area(BSA) was 18% and the body mass index (BMI) was 18.5 kg/m2.There was neither a previous history of diabetes mellitus nor a family history of hereditary disease.
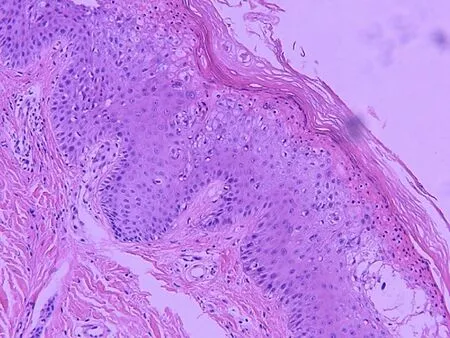
Fig. 1. Histology of the lesions. Atrophic epidermis can be seen with moderate spongiosis and a central area with marked pallor due to the presence of apoptotic and vacuolated keratinocytes below a superficial layer of extensive hyperkeratosis and parakeratosis (hematoxylin eosin staining, original magnification × 20).
The laboratory examinations showed the following results:hemoglobin 105 g/L; calcitonin angiotensinogen 4.32 ng/mL; fasting blood glucose 5.6 mmol/L; urine glucose 4 + ; and plasma glucagon 257 ng/L. Histopathology of the biopsied skin lesion showed epidermal hyperkeratosis and incomplete keratinization,necrosis of keratinocytes in the upper epidermis, and infiltration of a small amount of lymphocytes around the dermal vessels ( Fig. 1 ).
Contrast-enhanced computed tomography (CECT) of the abdomen revealed that the pancreatic head was enlarged (3.8 × 2.3 cm), with a poorly defined boundary and uneven enhancement on the enhanced scan ( Fig. 2 ). Magnetic resonance imaging (MRI)showed that the head of the pancreas was enlarged in shape, and a mass-like abnormal shadow (2.8 × 1.8 cm) was seen, with iso-/hypo-intense signals on T1WI, hyper-intense signals on T2WI, and hyper-intense signals on DWI ( Fig. 3 ). Dynamic enhancement scan revealed that the lesion was slightly enhanced, and the degree of enhancement was lower than that of the surrounding pancreatic tissue; the tail and the body of the pancreas were normal in shape,with no difference in signals. A space-occupying lesion at the head of the pancreas was considered.

Fig. 2. Contrast-enhanced computed tomography (CECT) of the abdomen revealed that the head of the pancreas was enlarged (3.8 × 2.3 cm), with a poorly defined boundary and uneven enhancement on the enhanced scan.
Pathology of the biopsied specimen revealed a small number of differentiated neuroendocrine tumor cells in the fibrin exudates,and the possibility of a highly-differentiated neuroendocrine tumor was considered. Other pathological findings included CK ( + ), Vimentin ( + ), CGA ( + ), SYN ( + ), CD56 ( + ), CD10 (-), PR ( + ), Gal3 (-),E-cadherin ( + ), CyclinD1 (-), and Ki-67 ( + ) ( Fig. 4 ).

Fig. 3. Magnetic resonance imaging (MRI) showed that the head of the pancreas was enlarged in shape, and a mass-like abnormal shadow (2.8 × 1.8 cm) was seen,with iso-/hypo-intense signals on T1WI, hyper-intense signals on T2WI, and hyperintense signals on DWI.
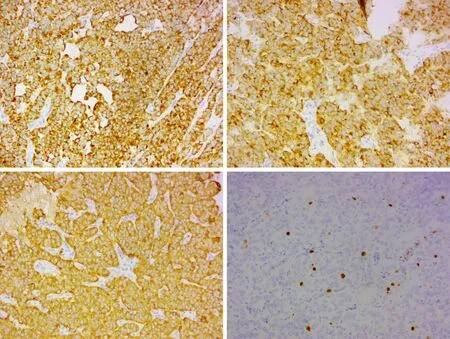
Fig. 4. Immunohistochemical studies on pancreatic section indicated CK ( + ), CGA ( + ), SYN ( + ), and Ki-67 ( + ) (original magnification × 200).
After adequate preoperative examinations, the patient underwent pancreaticoduodenectomy and peripancreatic nerve resection on June 25, 2016. During the surgery, a mass measuring 2.0 × 1.6 cm was observed at the head of the pancreas. The pathological findings of the surgically resected specimen were almost the same as the results of the pathology of biopsy specimen. No metastasis was seen in the perigastric lymph nodes. The final diagnosis was GS with NME. She has been followed up for 5 years, during which the rash resolved without recurrence, and rhagades and erosions in the perioral and lingual areas had subsided. She had normal diet,the BMI was 20 kg/m2, and the quality of life was improved significantly.
GS is a cutaneous paraneoplastic syndrome caused by a glucagon-secreting tumor derived from pancreatic isletαcells. GS can have a variety of systemic manifestations including decreased body mass (66%), NME (70%), diabetes mellitus (83%), labyrinthitis or stomatitis (34%), and anemia (43%-90%) [5-11] . Cutaneous manifestations are usually considered to be intermediate to late manifestations of glucagonoma [12] . In the present case, initial presentation was skin lesions. The patient presented with recurrent widespread erythema, papules, blisters, erosions, and exudates in the earlier stage. The patient also had stomatitis and reduced BMI(18.5 kg/m2) but had no diabetes or diarrhea. She was diagnosed with GS based on CECT findings and the pathological results of ultrasound-guided biopsy.
Glucose abnormalities in GS patients are mostly mild diabetes or abnormal glucose tolerance [13] . In this case, the previous blood glucose was basically normal, urine glucose was 4 + , and no abnormality in blood glucose or glucose tolerance was found during the perioperative and postoperative follow-up periods. It is generally believed that the gluconeogenic and pro-glycogenic effects of glucagon can lead to an increase in blood glucose; however,glucagon can also stimulate insulin secretion, thus weakening its glucose-raising effect [ 14 , 15 ]. In the present case, multiple tests for fasting blood glucose and insulin levels showed normal results,suggesting that even if the blood glucose is normal and the skin lesion is suspected of being NME, the possibility of GS should also be considered. For tumors at the head of the pancreas, although many patients with NME can also have glucagonoma, NME is only a paraneoplastic manifestation of pancreatic tumors. CT and MRI are useful in locating the tumors, whereas endoscopic ultrasoundguided biopsy is a minimally invasive technique and can offer accurate pathological evidence. Our patient underwent ultrasoundguided biopsy, and the pathological findings provided a basis for surgical resection.
Glucagonoma is one of the functioning pancreatic neuroendocrine tumors and its treatment mainly includes surgery and drug therapy [15] . Surgical resection remains the preferred treatment. Glucagonoma can be either benign or malignant, and it is usually found in the tail of the pancreas. It is generally believed that glucagonoma accompanied by NME is more likely to be malignant. A previous study showed that 62% of glucagonomas had liver metastases, although metastases to lymph nodes, bones,and adrenal glands were also detected [3] . Somatostatin analogues can be employed to treat slowly-progressing Gl and G2 neuroendocrine tumors as well as somatostatin receptor-positive G3 tumors, with few adverse effects [16] . Targeted therapy (e.g., sunitinib and everolimus) can also be used for advanced functional pancreatic neuroendocrine tumors [ 17 , 18 ]. In the present case, although the skin lesions had lasted up to 5 years, the tumor in the head of the pancreas was still small (2.0 × 1.6 cm) when the diagnosis of glucagonoma was confirmed. No metastasis was detected by preoperative imaging or during the operation, and histopathology showed benign changes (G2). The tumor was radically resected, and radiochemotherapy or targeted therapy was not applied according to related guidelines. No recurrence was noted during the 5-year follow-up.
In conclusion, although GS is an extremely rare condition, our case suggests that the possibility of GS should be ruled out in patients with periodic episodes of migratory annular or figurative dark red plaques accompanied by blisters, erosions, and crusting,even if the blood glucose is normal.
Acknowledgments
None.
CRediT authorship contribution statement
Wei-Fang Zhu: Funding acquisition, Investigation, Writing -original draft. Shu-Sen Zheng: Conceptualization, Writing - review& editing.
Funding
This study was supported by a grant from Zhejiang Provincial Natural Science Foundation of China (LGF21H190 0 04).
Ethical approval
Written informed consent for publication was obtained from the patient.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2021年6期
Hepatobiliary & Pancreatic Diseases International2021年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatocellular-cholangiocarcinoma with sarcomatous change:Clinicopathological features and outcomes
- Successful treatment of complete traumatic transection of the suprahepatic inferior vena cava with veno-venous and cardiopulmonary bypass with hypothermic circulatory arrest ?
- Successful withdrawal of antiviral treatment in two HBV-related liver transplant recipients after hepatitis B vaccination with long-term follow-up
- High perioperative lactate levels and decreased lactate clearance are associated with increased incidence of posthepatectomy liver failure
- An NSQIP survey of outcomes after resection of choledochal cysts in adults
- A rare type of choledochal cysts of Todani type IV-B with typical pancreaticobiliary maljunction
