Systematic review and meta-analysis of outcomes of anatomic repair in congenitally corrected transposition of great arteries
Arka Chatterjee,Neal J Miller,Marc G Cribbs,Amrita Mukherjee,Mark A Law
Abstract
Key words:Congenitally corrected transposition of great arteries;Anatomic repair;Double switch operation;Atrial switch Rastelli;Hemi-Mustard Rastelli;Atrio-ventricular block
INTRODUCTION
Congenitally corrected transposition of the great arteries(cc-TGA)is an uncommon cardiac defect accounting for less than 0.5% of congenital heart disease[1,2].Associated anatomic cardiac abnormalities include ventricular septal defects and pulmonary and subpulmonary obstruction,coarctation and Ebstein’s anomaly of the tricuspid valve(TV)[1].Surgical anatomic correction,depending on underlying associated cardiac anomalies,can be obtained with either a double switch operation(Senning/Mustard atrial switch and arterial switch)or an atrial switch(Senning/Mustard)with a Rastelli operation(ventricular septal defect closure with a baffle to the aorta and a right ventricle to pulmonary artery conduit).An additional variation includes a hemi-Mustard with a bidirectional Glenn shunt.The anatomic repairs allow for the left ventricle to become the systemic ventricle.This reduces the long-term deleterious risk of systemic right ventricular(RV)failure,and the propensity for progressive systemic TV insufficiency[3,4].
There are multiple long-term complications that can occur after anatomic repair for cc-TGA.Patients with cc-TGA are prone to developing atrioventricular block(AVB)requiring pacemaker implantation regardless of operative intervention[5,6].Furthermore,the baffles for systemic and pulmonary venous return have been shown to place patients at long-term risk for the development of atrial arrhythmia,though this risk might be mitigated by having a systemic left ventricle[6,7].Postoperative baffle leaks and stenoses are an additional complication that can lead to a variety of symptomology including cyanosis,paradoxical embolism,or venous congestion.Finally,the long-term transplant free survival remains unknown without comparison to survival following a physiologic repair strategy[8].
Anatomic repair for cc-TGA is the preferred treatment strategy for many institutions;however,the short and long-term outcomes are mostly limited to single center studies with a limited number of patients.We therefore sought to better delineate the short-term surgical outcomes and long-term risks including need for pacing,baffle complications requiring reintervention,symptoms,and transplant free survival by pooling the data from multiple observational studies.
MATERIALS AND METHODS
MEDLINE and Scopus databases were queried for manuscripts published till December 31,2017 with the search items“transposition great arteries”;“TGA”;“double switch”and“anatomical repair”.All manuscripts reporting outcomes of anatomic repair in cc-TGA patients were considered in the initial review.Final inclusion criteria were a minimum sample size of 5 patients with at least 2 years of follow up.Many centers have published multiple reports of their experience at varying follow up durations.Thus,the most up to date manuscript from each group was selected.Two authors(Chatterjee A and Law MA)independently reviewed all studies considered to ensure no overlap amongst included studies.Figure 1 shows the relevant details of the study selection process.
Full texts for all potentially relevant studies were extracted and examined for alignment with inclusion criteria and verification of outcomes reported.All initially considered studies were discussed formally amongst experienced cardiologists(Chatterjee A,Cribbs MG,Law MA)and a final list was drawn up.Relevant data was then extracted from these manuscripts and reviewed for accuracy by two authors(Law MA,Chatterjee A)independently.Any disagreement was discussed in the group for resolution.
Primary outcome studied was operative mortality of the anatomic repair strategy.We also evaluated immediate operative complications including the need for extra corporeal membrane oxygenation(ECMO)or left ventricular assist devices(LVAD)and AVB requiring a pacemaker.Long term outcomes evaluated were transplant free survival,New York Heart Association(NYHA)class of patients,need for pacemaker,and rate of re-interventions.We also pooled data for development of left ventricular(LV)systolic dysfunction:LV dysfunction was defined as LV ejection fraction <40% or when reported as moderate or severe.
Comprehensive meta-analysis(version 3;Biostat,Englewood,NJ)software was used to perform the meta-analysis.Short-term outcomes are reported as events(%)and long-term outcomes or reinterventions are reported as events per 100 patient years(PY).Heterogeneity in the data was assessed with theI2test(I2>50 and Cochran’s Q statisticPvalue <0.05 implying significant heterogeneity)[9].Random effects modelling was used in keeping with the observational nature of the reports included and also heterogeneity.Publication bias was assessed using the standard funnel plot method using standard errors and any corrections assessed using the Duvall and Tweedietrim and fillmethod.Two-tailedPvalues were used withP<0.05 implying statistical significance and confidence intervals(CI)were reported at the 95% level.PRISMA guidelines were followed in reporting the meta-analysis results[10].
RESULTS
Twenty-one reports of anatomic repair were included in the final analysis[4,11-30].Table 1 lists the studies included and the type of anatomic repair used.A total of 895 patients with cc-TGA underwent anatomic repair:The pooled analysis yielded a total follow up of 5457.2 PY.The median/mean age at operation varied from 0.75–11.1 years.Four hundred and thirteen patients underwent the double switch operation(DS)while 482 patients underwent either an atrial switch-Rastelli operation or a hemi-Mustard Glenn-Rastelli operation(ASR).Sixteen studies reported patients with both types of operations;4 studies reported experience with ASR operations only and 1 study reported only DS outcomes.Fifteen studies reported prevalence of moderate or more tricuspid regurgitation(TR):22.7%(150/677)of the pooled sample had significant TR.Fifteen studies reported data on pre-existing AVB:This reveals that 15.6%(104/667)patients have a need for pacing even before any surgical repair.
Short term outcomes
A total of 64 patients did not survive to discharge after initial operation giving a pooled estimate for operative mortality of 8.3%(95%CI:6.0%-11.4%).Figure 2 shows the funnel plot for operative mortality for included studies which would suggest overreporting of small studies with low operative mortality.Correcting for publication bias would raise the estimate of operative mortality to 10.9%(CI:7.6%-15.5%).Need for mechanical circulatory support with ECMO / LVAD post operatively was 0.2%(CI:0.1%-0.4%).Only 1.7%(CI:1.1%-2.4%)patients developed AVB needing implantation of a permanent pacemaker.
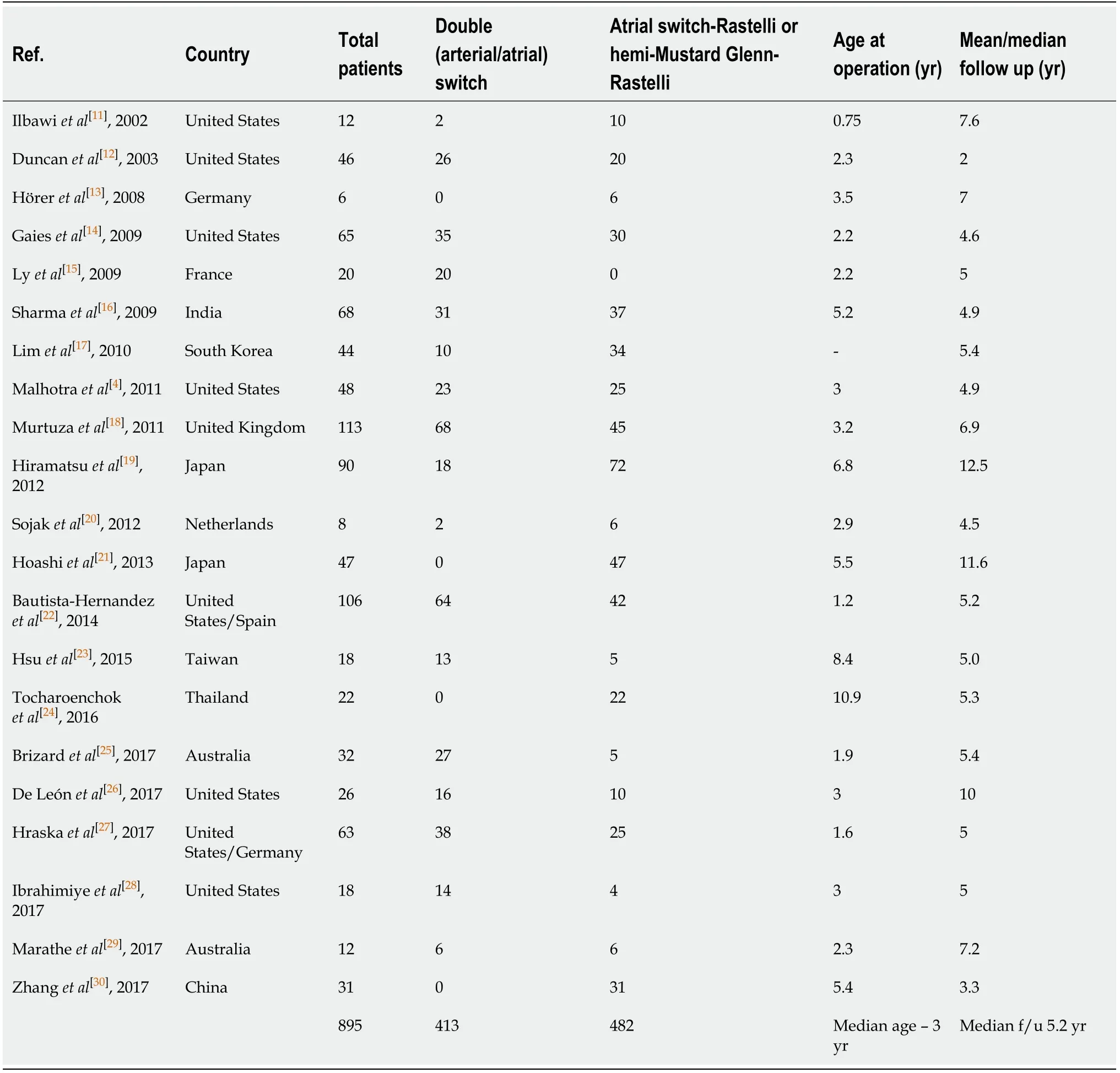
Table 1 Baseline characteristics of included studies
Follow up outcomes
Long term outcomes are tabulated in Table 2.In patients surviving the initial operation,mortality(Figure 3)was estimated to be 0.6 per 100 PY(CI:0.4-0.8).Fourtyeight patients died over the cumulative follow up of 5457.2 PY.In 20 studies that reported need for transplantation,10 patients underwent heart transplantation giving an estimated overall survival free of death or needing transplant of 92.5%(CI:89.5%-95.4%)per 100 PY.Thirteen studies reported data on functional class of surviving patients:84.7%(CI:79.6%-89.9%)patients were estimated to be in NYHA functional class I or II.Eighteen studies reported data on LV systolic function in long term follow up and LV dysfunction was estimated to happen in 1.7 patients/100 PY(CI:1.0%-2.4%).
In long term follow up,further need for pacemaker was noted to be 0.3%/100 PY;(CI:0.1%-0.4%).
Re-interventions
Twenty studies reported data on total re-interventions and the pooled estimate was 5.3 per 100 PY(CI:3.8-6.8)with incidence of baffle stenosis being estimated to be 1.1(CI:0.8%-1.5%)/100 PY.The most frequently needed reoperations/reinterventions were for conduit replacements or rehabilitation(1.5/100 PY;CI:0.9-2.1).
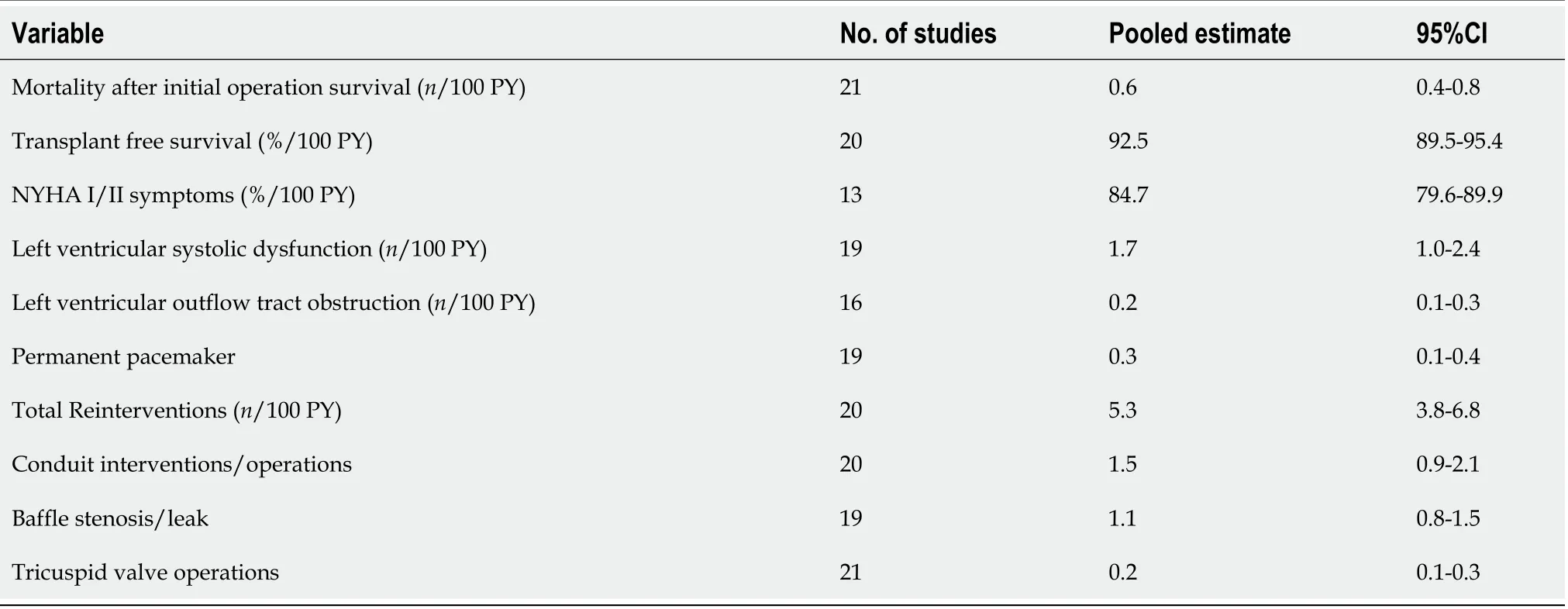
Table 2 Outcomes of anatomic repair in long term follow up
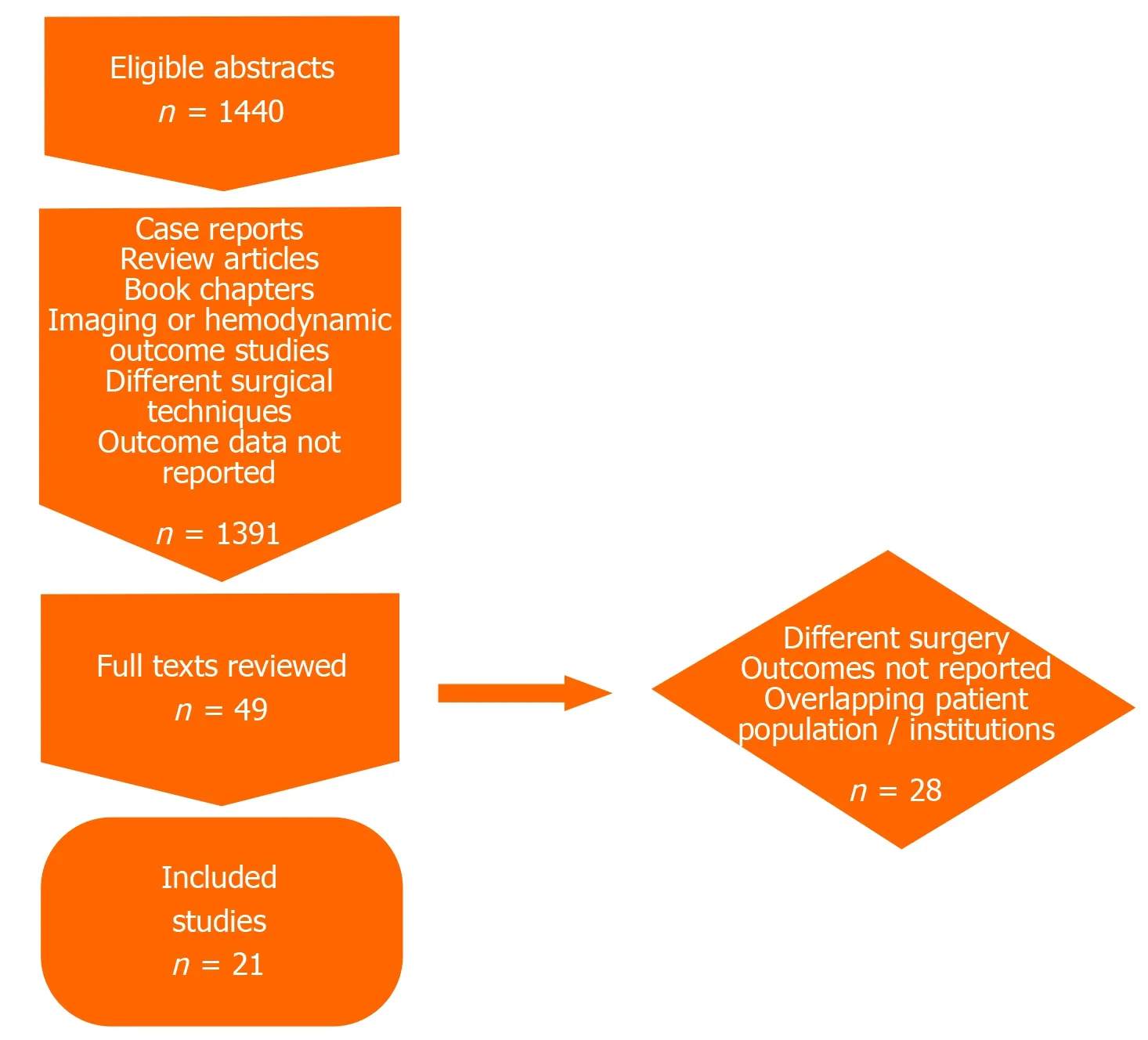
Figure 1 Flowchart depicting study selection process.
DISCUSSION
This is a thorough attempt to use a meta-analysis study design in order to estimate the long-term outcomes with an anatomic repair strategy in this rare congenital heart disease subset.We report pooled outcomes from 895 patients with a sizeable follow up of >5000 PY.Management patterns for patients with cc-TGA are dictated by variations in anatomic substrate and often by the experience of individual centers[3].The longterm outcomes with a physiologic repair strategy keeping the right ventricle as the systemic ventricle,although considered safe unmistakably leads to progressive congestive heart failure.Grahamet al[31]report that 67% patients with ccTGA and associated abnormalities develop congestive heart failure by age 45 and Hraskaet al[32]estimate the 10-year survival after physiologic repair to be 68% only.With a low follow up mortality of 0.6/100 PY in a very large pooled sample,our results would certainly argue for anatomic repair being a default strategy for patients unless the substrate is not suitable.Most reports of anatomic repair would identify this unsuitable group as older patients whose morphological LV may not be able to sustain systemic pressures or not respond to training with a pulmonary artery band[33].Other predictors of poor outcomes after anatomic repair are significant pre-existing TR,RV dysfunction and need for pacing[17,22].
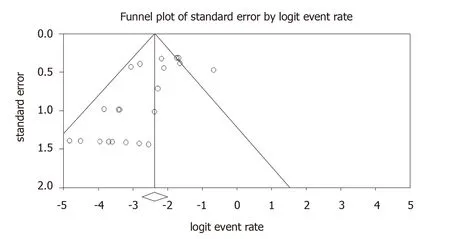
Figure 2 Funnel plot for operative mortality after anatomic repair for congenitally corrected transposition of great arteries showing publication bias to the left of mean.
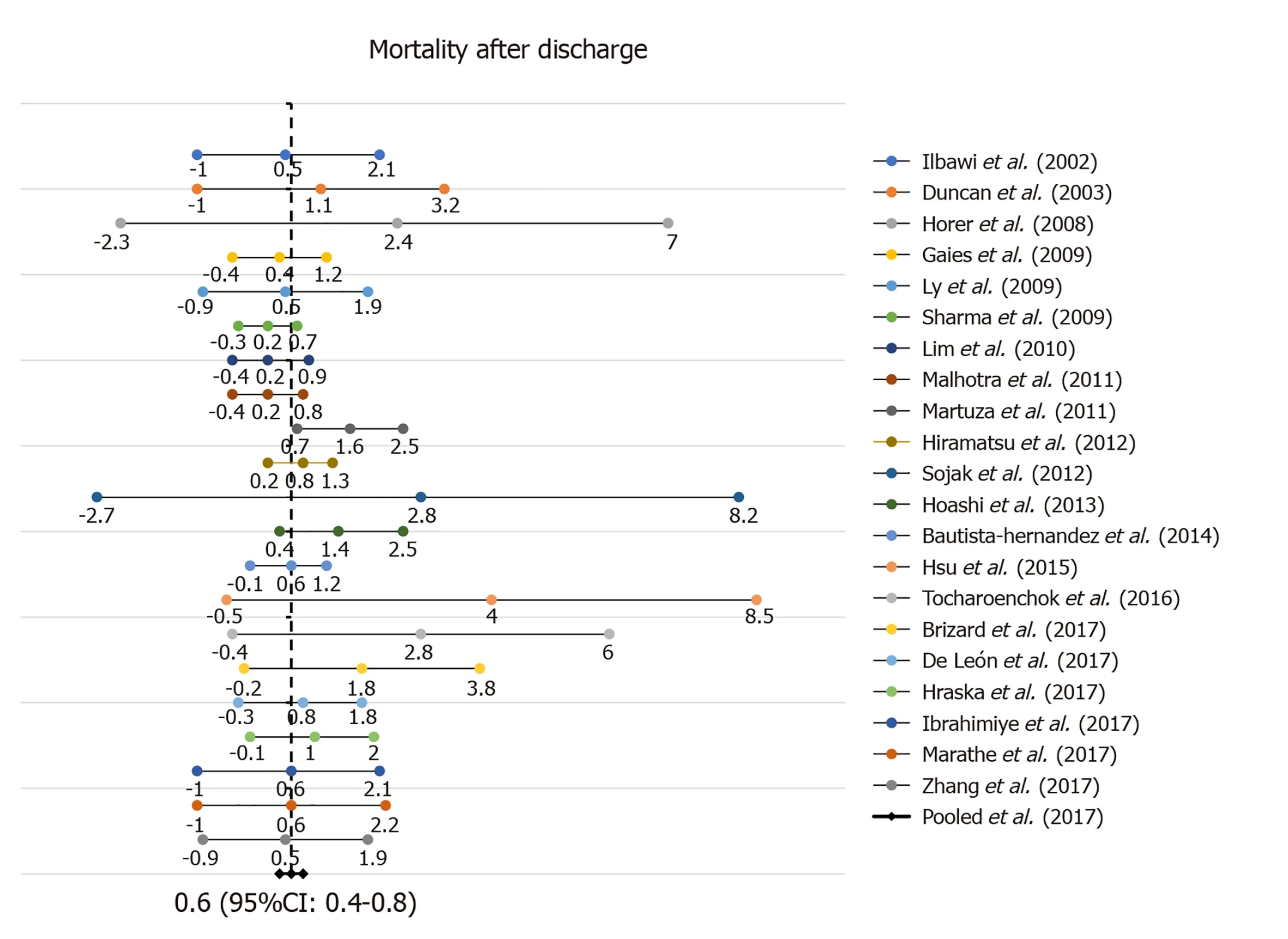
Figure 3 Forest plot for long term mortality after anatomic repair for congenitally corrected transposition of great arteries.CI:Confidence interval.
This improved longer term survival outcome over physiological repair needs to be weighed over the apparent short-term safety of only correcting associated abnormalities in a physiologic repair strategy[34].However,the surgical mortality in physiologic repair population is also not negligible,being reported at 3% in operations done after 1986 in a Mayo Clinic series(16% overall)and 6.7% in the Dutch series by Bogerset al[35,36].The operative mortality in our pooled sample is slightly higher than previously reported estimates[37].However,this is also a sample with a greater proportion of DS operations versus ASR operations.This is notable since multiple reports have considered the latter to have lower risk of operative mortality[38].
Staged single ventricle palliation with Fontan completion has been advocated as an alternative strategy in the management of cc-TGA[29,39].The short-term results are comparable in regard to survival and symptomatology,but one must consider that long-term complications are not trivial with many patients experiencing morbid complications.In a study by Denniset al[40],survival of patients was only 80% at the age of 40 years with many patients experiencing arrhythmia,embolic complications,and cardiac failure only after 16 years of age.
AVB in this population is consistently associated with poor outcomes[6].However,our study results suggest that operative strategy may not make a huge incremental difference in the development of AVB.The post-operative need for pacing was only 1.7% with the long-term additional need for pacing in another 0.3% patients only.
Re-interventions after anatomic correction for cc-TGA are not rare as corroborated by our analysis.Especially in the ASR cohort,conduit replacements are very common and likely most patients will need at least one exchange to a larger conduit suitable for transcatheter replacement.However,after the first reoperation,multiple transcatheter replacements or rehabilitation procedures can be done avoiding the need for reoperation[41,42].
Baffle complications of residual leaks or stenosis are well described after the Mustard/Senning operations and thus account for the other common reoperations after anatomic repair for cc-TGA[43].However,in the current era,most of the baffle related complications can be adequately managed with transcatheter techniques minimizing the need for re-operations[44,45].Furthermore,residual LVOT obstruction is known after both types of anatomic repair[46].Our analysis shows the incidence of this is low but not completely negligible.
However,the need for re-interventions should also be noted in the context of similar or higher need for reoperations and reinterventions in the physiologic repair strategy.In a sample of 111 children who underwent physiologic repair only,41% patients required reoperations for conduit exchanges or TV repair/replacement at a mean follow up duration of 11.4 years[36].Similarly,Bogerset al[35]have also reported a reintervention rate of 32% at 20 years with a physiologic repair.
Limitations
The meta-analysis study design lends itself to certain characteristic limitations.Systematic pooling of observational studies with differences in baseline patient characteristics,varied anatomic substrate,different sample sizes,surgical technique and different follow-up durations make the pooled sample more heterogenous.This is also not a patient level meta-analysis which can overcome some of these limitations.In congenital heart disease literature,reports often consist of small sample sizes and limited follow up,hence pre-disposing to lower than actual pooled estimates when included in a meta-analysis.Since all the studies included are observational,there is also the consideration of under-reporting of outcomes or exclusion of patients with poor outcomes.There is also no way to adequately account for refinement in surgical technique as experience with anatomic repair grew.
Conclusion
This large pooled analysis supports the overall favorable outcomes after anatomic repair for cc-TGA,especially beyond the early initial operative period.Majority of patients have good quality of life,falling in NYHA class I or II.Despite increase in the complexity of repair,there does not seem to be a large increase in the prevalence of heart block.Re-interventions are required but can be accomplished in many situations with transcatheter techniques in the modern era.
ARTICLE HIGHLIGHTS
Research background
Anatomic repair for congenitally corrected transposition of great arteries(cc-TGA)is accomplished by either a double switch operation or one of many modifications of an atrial switch operation combined with a Rastelli operation.However,these operations are complex and a simpler physiologic repair strategy of correcting only associated defects like tricuspid valve regurgitation or ventricular septal defects is also adopted in many patients.Anatomic repair strategy has the benefit of restoring the left ventricle to the systemic circulation,thus decreasing the chances of development of congestive heart failure from a systemic right ventricle.
Research motivation
There are variations in practice regarding anatomic versus physiologic repair for cc-TGA.Long term data from a large set of patients regarding safety and outcomes of anatomic repair are lacking.
Research objectives
The objective of this study was to pool high quality observational studies reporting outcomes after anatomic repair in cc-TGA patients and perform a systematic review and meta-analysis to provide more comprehensive outcomes.
Research methods
A search of MEDLINE and Scopus was conducted using pre-defined search criteria to identify manuscripts reporting outcomes after anatomic repair.Studies meeting inclusion criteria were reviewed and information regarding variables of interest were extracted.Meta-analysis was performed according to standard methods using Comprehensive meta-analysis software(version 3).
Research results
Eight hundred and ninety-five patients who were treated with an anatomic repair strategy were pooled from 21 studies with a total follow-up of 5457.2 patient-years(PY).Estimated operative mortality was 8.3%.Survivors had a transplant free survival of 92.5%(CI:89.5%-95.4%)per 100 PY.84.7% patients experienced a New York Heart Association functional class I or II after 100 PY follow up.There were 5.3 reoperations/re-interventions per 100 PY(CI:3.8-6.8).
Research conclusions
Our study reports a high operative mortality rate for anatomic repair strategy in cc-TGA patients.However,the long-term survival is excellent for survivors.
Research perspectives
Our study suggests that the anatomic repair is worth pursuing in most patients with cc-TGA because of favorable long-term outcomes despite a high operative mortality risk.Re-intervention/reoperation risk remains – however with the advent of transcatheter therapies,most of these issues can be managed without a re-operation in the modern era.
 World Journal of Cardiology2020年8期
World Journal of Cardiology2020年8期
- World Journal of Cardiology的其它文章
- Oliver Wendell Holmes’1836 doctorate dissertation and his journey in medicine
- Impact of cardiologist intervention on guideline-directed use of statin therapy
- Forensic interrogation of diabetic endothelitis in cardiovascular diseases and clinical translation in heart failure
- Sympathetic nervous system activation and heart failure:Current state of evidence and the pathophysiology in the light of novel biomarkers
- Classic Ehlers-Danlos syndrome and cardiac transplantation-Is there a connection?
