Postpartum Atypical Hemolytic Uremic Syndrome: an Unusual and Severe Complication Associated with IgA Nephropathy
Li-xian Sun, Wen-ling Ye*, Yu-bing Wen, and Xue-mei Li
1Department of Cardiology,2Department of Nephrology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
Postpartum Atypical Hemolytic Uremic Syndrome: an Unusual and Severe Complication Associated with IgA Nephropathy
Li-xian Sun1, Wen-ling Ye2*, Yu-bing Wen2, and Xue-mei Li2
1Department of Cardiology,2Department of Nephrology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
acute kidney injury; hemolytic uremic syndrome; IgA nephropathy; pregnancy
Chin Med Sci J 2015; 30(3):189-192
IGA nephropathy (IgAN) is one of the most common types of primary glomerulonephritis, which occurs more frequently in patients of reproductive age. Atypical hemolytic uremic syndrome (aHUS)
without diarrhea is rare and has a poor prognosis. In the absence of appropriate therapy, pregnancy-related aHUS is associated with high morbidity and mortality. This report described a successfully treated case of postpartum aHUS associated with IgAN. Repeated renal biopsy was performed to demonstrate serial renal pathologic changes after successful treatment.
CASE DESCRIPTION
A 26-year-old female (gravida 1, para 1) presented with acute kidney injury (AKI), nephrotic syndrome, thrombocytopenia and hemolytic anemia 5 days after delivery. Routine urinalysis showed protein (1-2+) and blood (2-3+) at the 22ndgestational week. Her blood pressure remained normal during the pregnancy, and her medical history was negative before gestation.
Five days after cesarean section in the 40thgestational week, her urine volume started to decline, her blood pressure increased with maximum measurement at 180/110 mm Hg, and she developed progressive AKI. She had no fever, nor abnormality on neurological examinations. Her platelet count dropped to a minimum of 48×109/L, and hemoglobin to 80 g/L with red blood cell fragmentation in peripheral blood smears. Her urinary protein excretion was 6.24 g/day. Serum biochemical parameters revealed low albumin (18 g/L) and total protein (32 g/L) and elevated lactate dehydrogenase (1324 U/L). Her alanine aminotransferase, aspartate aminotransferase, immunoglobulin and serum complement concentrations were normal. The detection for antinuclear antibodies (ANA), lupus anticoagulant and anticardiolipin antibody was negative.
The diagnosis of HUS was made and she was treated with intravenous methylprednisolone (60 mg/day) and fresh frozen plasma infusion (400-600 ml/day) for 1 week, followed by oral methylprednisolone [0.8 mg/(kg·d)]. Hemodialysis three times per week was initiated when her serum creatinine was measured at 521 μmol/L one week after delivery. Her platelet count gradually increased to (80-100)×109/L and her blood pressure was controlled atlower than 140/90 mm Hg by angiotensin-converting enzyme inhibitors and angiotensin receptor blocker. A percutaneous renal biopsy was performed 2 weeks after delivery. Immunofluorescence showed intense (3+) staining for IgA and C3 in the mesangial area (Fig. 1A). Light microscopy displayed severe mesangial proliferation and typical lesions of thrombotic microangiopathy (TMA), including subendothelial mucosal edema, fibro-necrosis and marked thickening of the artery walls in the majority of afferent arterioles and interlobular arteries (Fig. 1 B, C). The lumen of most arterioles was nearly completely occluded.
Her renal function partially improved after 6 weeks of treatment, when hemodialysis and methylprednisolone were discontinued. She was referred to our hospital 7 months after delivery because of sustained nephroticrange proteinuria and renal dysfunction. Laboratory tests showed blood (3+) in urine, proteinuria of 3.21 g/24 h, hemoglobin of 104 g/L, platelet count of 239×109/L, and serum creatinine concentration of 143 μmol/L. Repeated renal biopsy showed moderate mesangial hypercellularity with segmental sclerosis and ischemic glomerular lesions (Fig. 1 D-F). Immunofluorescence findings were comparable with those observed during the first biopsy. She was prescribed with prednisone [1 mg/(kg?d)], which was decremented gradually after 6 weeks and maintained with the dose of 5 mg/day for 1 year. She was also administered oral cyclophosphamide (100 mg/d) with cumulative dosage of 9 grams. Her serum creatinine concentration decreased to 110-120 μmol/L, and her 24-hour urinary protein was less than 1 g in the follow-up visits after one year.
DISCUSSION
HUS, a form of TMA characterized by thrombocytopenia, hemolytic anemia and AKI, is a life-threatening disorder presenting in 2.3%-9.1% of obstetric women with AKI.1,2In contrast to typical HUS, which is associated with diarrhea, aHUS, which occurs without diarrhea, is rare and has a poorer prognosis. It is usually secondary to autoimmune disease, malignant hypertension or medication.3Pregnancy is also a risk factor for aHUS, with the highest incidence near term and during the postpartum period. This is also the time of greatest risk for thrombotic events and for the occurrence of other pregnancy-related syndromes: preeclampsia, eclampsia, and hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome.4
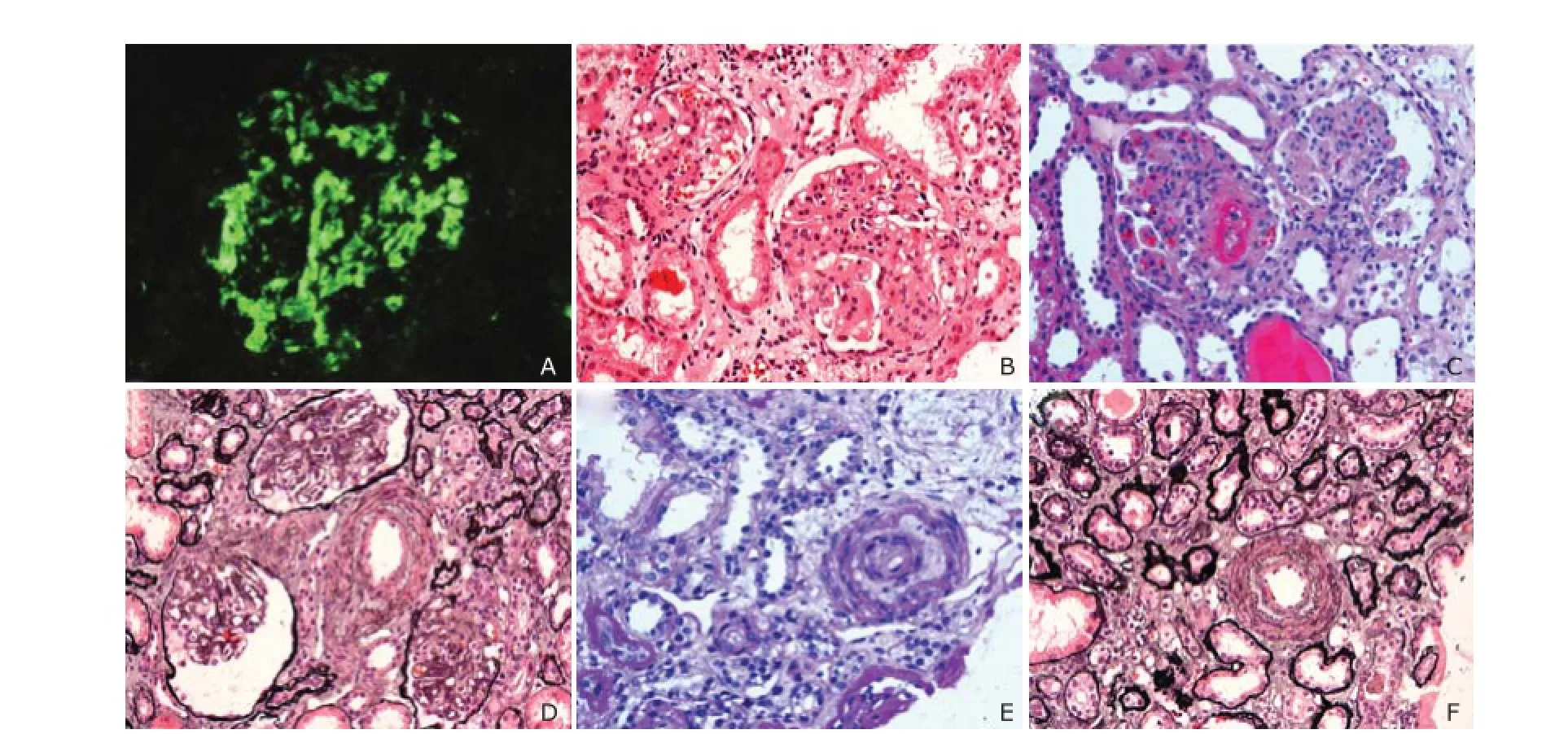
Figure 1. Serial renal pathologic changes 2 weeks and 7 months after delivery.A. Immunofluorescence showing diffuse and massive deposits of IgA in the mesangial area, confirming the diagnosis of IgA nephrology (×400).B. First renal biopsy performed 2 weeks postpartum, showing fibrinoid necrosis in the afferent arterioles. The glomerulus display severe mesangial proliferation and intracapillary thrombi (periodic acid-schiff stain, ×200).C. Renal biopsy at 2 weeks postpartum, showing severe mucosal edema with almost entirely occluded lumen in the interlobular (periodic acid-schiff stain, ×200).D-F. Renal biopsy taken 7 months after delivery, revealing moderate mesangial hypercellularity with mesangial expansion and segmental sclerosis (D, HE, ×200) and enlargement of the Bowman capsule (E, PASM, ×200). The vascular lumen of the interlobular arteries being re-canalized with mild intimal elastic membrane thickening (E&F, PASM, ×200).
Although IgAN is one of the most common primary glomerulonephritis, its diagnosis can only be confirmed by the immunolocalization of mesangial IgA deposition. Pregnancy-related aHUS is quite rare in the setting of IgAN. A search in Medline using the keywords “pregnancy”,“hemolytic uremic syndrome” and “IgAN” yielded no articles published between 1966 and 2013. The incidence of aHUS associated with IgAN may be underestimated because some pregnant women with aHUS have no opportunity to renal biopsy with the contraindication of severe illness or continuous thrombocytopenia. The strong deposition of IgA in mesangial areas and pathological findings typical of mesangial proliferation confirmed the diagnosis of IgAN in this case. Routine examination during the pregnancy showed microhematuria and proteinuria without hypertension, which is the most common manifestation of IgAN, indicating that this patient had developed IgAN before aHUS.
Pregnancy-related HUS has a very poor prognosis, with a maternal mortality rate of 44% and a perinatal mortality rate of 80%.5Although the standard treatment of aHUS associated with IgAN is uncertain, early plasma exchange, plasma infusion, and glucocorticoids are considered effective and have been associated with a favorable outcome.6Fortunately, the hemolytic anemia, thrombocytopenia, and renal dysfunction in this case were rapidly ameliorated after plasma infusion, glucocorticoid therapy, and hemodialysis. Sustained nephrotic-range proteinuria and hypoalbuminemia, confirmed by repeated renal biopsy, was further improved after prescription of prednisone and cyclophosphamide and her renal dysfunction was gradually ameliorated.
The pathogenesis of postpartum aHUS occurring in IgAN is not well understood. Several causes or triggering factors may be involved in this process. Hypercoagulable state caused by nephrotic syndrome and pregnancy was substantially considered to be an important risk factor for aHUS. TMA was found to be associated with severe proteinuria in patients with IgAN.7This patient presented with nephrotic syndrome with very severe hypoalbuminemia (18 g/L) when HUS developed. Nephrotic syndrome may contribute to thrombus formation in arterioles due to increased procoagulation factors, decreased anticoagulation proteins and fibrinolytic precursors.8Pregnancy is also associated with increases in coagulation factor levels and decrease in natural anticoagulation, leading to a hypercoagulable state with the greatest abnormalities at term and perinatal period. Thus, the combined effect of these two conditions leads to an increased tendency of thrombosis. In addition, severe mesangial proliferation of IgAN, as in this patient, may result in further injury of endothelial cells of glomerular capillaries by the deposition of IgA immune complexes at subendothelium, expansion of the mesangial matrix, and mesangial cells proliferating into the subendothelium.
Recently, genetic abnormalities of complement regulatory genes are regarded as one of pathogenic mechanisms of aHUS.9,10A review of 21 pregnant French women with aHUS found that 18 of them had complement abnormalities and 17 had dysregulation of alternative complement regulatory proteins.10However, the involvement of the complement pathway in HUS development in this case is uncertain, since her complement level was normal at the time of HUS diagnosis. Several mechanisms may contribute to the association between aHUS and IgAN in this patient, including hypercoagulable state and oxidative stress caused by nephrotic syndrome, severe hypertension, mutations of genes encoding regulators of the alternative complement pathway, and high coagulation activity related to pregnancy. However, further investigations and researches are requisite to explore the exact mechanisms of aHUS.
In conclusion, although aHUS is rarely associated with IgAN, it should be considered in pregnant women with underlying glomerulonephritis when AKI occurs. Renal biopsies should be performed to exclude concomitant glomerulonephritis and titrate the appropriate therapy strategies for aHUS patients, especially in those with a history of microhematuria and proteinuria.
1. Silva GB Jr, Monteiro FA, Mota RM, et al. Acute kidney injury requiring dialysis in obstetric patients: a series of 55 cases in Brazil. Arch Gynecol Obstet 2009; 279: 131-7.
2. Hassan I, Junejo AM, Dawani ML. Etiology and outcome of acute renal failure in pregnancy. J Coll Physicians Surg Pak 2009; 19: 714-7.
3. Loirat C, Frémeaux-Bacchi V. Atypical hemolytic uremic syndrome. Orphanet J Rare Dis 2011; 6:60.
4. George JN. The association of pregnancy with thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Curr Opin Hematol 2003; 10: 339-44.
5. McCrae KR, Cines DB. Thrombotic microangiopathy during pregnancy. Semin Hematol 1997; 34: 148-58.
6. Elliott MA, Nichols WL. Thrombotic thrombocytopenic purpura and hemolytic uremic syndrome. Mayo Clin Proc 2001; 76: 1154-62.
7. Chang A, Kowalewska J, Smith KD, et al. A clinicopathologic study of thrombotic microangiopathy in the setting of IgA nephropathy. Clin Nephrol 2006; 66: 397-404.
8. Kerlin BA, Ayoob R, Smoyer WE. Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin J Am Soc Nephro 2012; 7: 513-20.
9. Leban N, Aloui S, Touati D, et al. Atypical hemolytic uremic syndrome in the Tunisian population. Int Urol Nephrol 2011; 43: 559-64.
10. Fakhouri F, Roumenina L, Provot F, et al. Pregnancyassociated hemolytic uremic syndrome revisited in the era of complement gene mutations. J Am Soc Nephrol 2010; 21: 859-67.
NOTICE OF RETRACTION
The Editor retracts the following article from Chinese Medical Sciences Journal:
Liu K, Hao J, Shi J, Dai C, Guo X. Blood Lead Levels During Pregnancy and Its Influencing Factors in Nanjing, China. Chin Med Sci J 2013; 28(2): 95-101.
The first author, Kang-sheng Liu, admitted to the editors to flaws in data collection and analysis that affect the authenticity and accuracy of this article. Dr Liu takes full responsibility for this.
Received for publication July 3, 2014.
*Corresponding author Tel: 86-10-69155058, E-mail: wenlyepumch@ 163.com
 Chinese Medical Sciences Journal2015年3期
Chinese Medical Sciences Journal2015年3期
- Chinese Medical Sciences Journal的其它文章
- Paraneoplastic Dermatomyositis Accompanying Nasopharyngeal Carcinoma
- Genetic Effects on Sensorineural Hearing Loss and Evidence-based Treatment for Sensorineural Hearing Loss
- Serum Myeloperoxidase Level in Systemic Lupus Erythematosus
- Pulmonary Carcinosarcoma with Intracardiac Extension: a Case Report
- Double Roots of Mandibular Premolar in Full-mouth Periapical Films
- Cerebrospinal Fluid Biomarkers in Dementia Patients with Cerebral Amyloid Angiopathy
