Clinical Study on Suspension Pancreatic-Duct-Jejunum End-to-Side Continuous Suture Anastomosis in Pancreaticoduodenectomy
Ke Dong,Wei Xiong,Xiao-jiong Yu*,and Chun Gu
Department of Hepatopancreatobiliary Surgery,Sichuan Provincial Academy of Medical Sciences &Sichuan Provincial People’s Hospital,Chengdu 610072,China
PANCREATICODUODENECTOMY (PD) was a classical operation performed to treat cancerous tumours in the head of the pancreas and periampullary cancer.However,due to its long operation time,combined resection of several vitals (including stomach,duodenum,upper jejunum,and pancreatic head),and reconstruction of gastrointestinal tract,PD is associated with several postoperative complications,among which one of the severest is pancreatic fistula.1-4Many factors affect the incidence of pancreatic fistula,such as the skills of the surgeon and the type of pancreaticojejunostomy,in which the only controllable factor is the type of anastomosis.4-8Based on clinical practice,the surgical team of Department of Hepatopancreatobiliary Surgery of Sichuan Provincial People’s Hospital has developed a new type of pancreaticojejunostomy that we named“suspension pancreatic duct-jejunum end-to-side continuous suture anastomosis (SPDJCS)”,achieving satisfactory clinical outcome.To evaluate the efficacy of this type of anastomosis in preventing post-PD pancreatic fistula,as well as its practicality and safety,a prospective non-randomized controlled study was conducted based on the clinical data of PD cases from January 2010 to May 2012.
PATIENTS AND METHODS
Patients
From January 2010 to May 2012,165 cases treated with PD were divided into 3 groups (group A,B,and C) according to the difference in anastomosis types.The patients were fully informed of the study and had signed informed consent forms before the grouping.The surgeons for each group were the same throughout this study.
Group A (end-to-end/end-to-side invaginated anastomosis) included 52 cases,with 36 males and 16 females,aged 51.2±17.2 years (31-73 years);45 cases with icterus and 21 cases with hypoproteinemia;3 cases of benign lesions in the head of the pancreas,including 1 case of cystadenoma and 2 cases of mass-type chronic pancreatitis (MTCP).
Group B (end-to-side mucosal anastomosis) included 48 cases,with 34 males and 14 females,aged 50.3±16.4 years (34-72 years);38 cases with icterus and 19 cases with hypoproteinemia;2 cases of MTCP in the head of the pancreas.
Group C (SPDJCS) included 65 cases,with 45 males and 20 females,aged 51.8±15.3 years (30-74 years);50 cases with icterus and 28 cases with hypoproteinemia;4 cases of benign lesions in the head of the pancreas,with 1 case of cystadenoma and 3 cases of MTCP.
All the patients in the three groups underwent preoperative examinations (computed tomography and/or magnetic resonance cholangiopancreatography).There was no significant difference (P>0.05) among the three groups in age,ratio of benign tumour cases to malignant tumour cases,and the preoperative levels of albumin,diabetes,hemoglobin,total bilirubin,and alanine amino transferase (Table 1).Neither was there difference (P>0.05) among the three groups in the clinical stage,the size of the pancreatic duct,and the texture of the pancreas are concerned (Table 2).
Methods of pancreaticojejunostomy
Group A∶An external drainage tube was inserted into the pancreatic duct,and into the jejunum through choledochojejunostomy stoma while the drainage tube remained in the body.4,5support through jejunal nutrient canal 48-72 hours after the operation.Patients diagnosed as developing pancreatic fistula were treated accordingly.
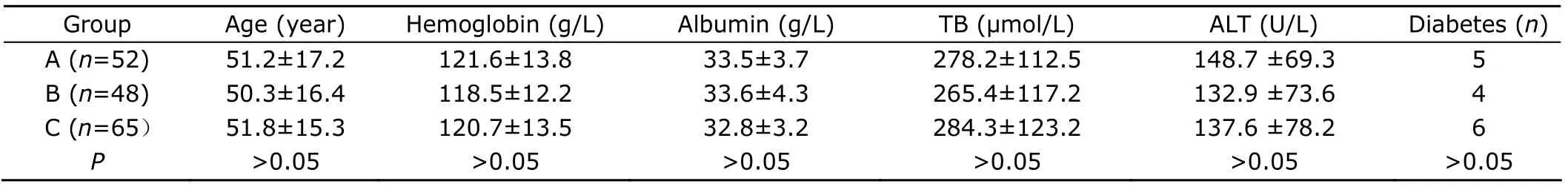
Table 1.Preoperative clinical data of patients in Groups A,B,and C§
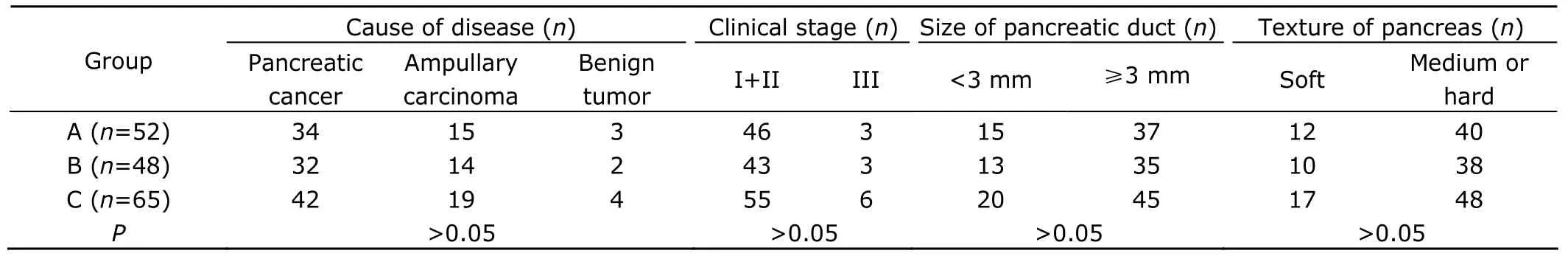
Table 2.Intraoperative clinical data of patients in Groups A,B,and C
Grading standard of pancreatic fistula
Among various grading standards for pancreatic fistula nowadays,the grading standard put forward by The International Study Group on Pancreatic Fistula (ISGPF) is widely accepted for its reasonableness.10-13This standard defines that pancreatic fistula could be diagnosed if concentration of diastase in the peritoneal drainage flow is 3 times higher than the concentration of serum amylase 3 days after the operation.Pancreatic fistula is classified into grades A,B,and C based on its clinical influence on the patients.Grade A is temporary pancreatic fistula accompanied by increased pancreatin in the drainage flow but no clinical symptoms.Grade B is pancreatic fistula with fever,abdominal pain,vomiting,abdominal signs,incapability of eating,and peripancreatic effusion.Grade C is pancreatic fistula with worse clinical symptoms and more obvious peripancreatic effusion compared with Grade B.13-15
Statistical analysis
The statistical analysis was performed with SPSS 11.5.The data were expressed in frequency and percentage,analyzed usingχ2test.P<0.05 was considered statistically significant.
RESULTS
The total incidence of pancreatic fistula was 13.9%(23/165),which was 23.1% (12/52) in Group A,18.8%(9/48) in Group B,and 3.1% (2/65) in Group C,the lowest among the 3 groups (P<0.05,Table 3).Among the 12 patients who developed pancreatic fistula in Group A,6 were classified into grade A pancreatic fistula,4 into grade B,and 2 into grade C.Among the 9 patients with pancreatic fistula in Group B,5 were in grade A pancreatic fistula,3 in grade B,and 1 in grade C.The 2 patients with pancreatic fistula in Group C were all classified into grade A.Group C had significantly better results than Groups A and B in operation time,volume of intraoperative blood loss,and amount of postoperative peritoneal drainage flow (P<0.05),while no significant difference was noticed between Group A and Group B (P>0.05).In respect of complications other than pancreatic fistula such as peritoneal hemorrhage,peritoneal abscess,delayed gastric emptying,pulmonary infection,and postoperative infection,there was no significant difference among the three groups (P>0.05).One case of perioperative death occurred in Group A due to peritoneal hemorrhea (Table 3).
DISCUSSION
Among all the complications of pancreaticoduodenectomy,one of the most common and severe was pancreatic fistula,with an incidence of 5%-40%.1The mortality caused by secondary peritoneal infection and hemorrhea as a result of corrosion of large vessels,both triggered by pancreatic fistula,was as high as 20%-50%.2There are many factors influencing the incidence of pancreatic fistula,including age,size and texture of the pancreas,diameter of the pancreatic duct,preoperative nutriture,bilirubin level,and above all,the type of pancreaticojejunostomy,the only controllable factor.Therefore,it is an urgency to improve the technique of pancreaticojejunostomy.The authors of this artide have created a new type named“suspension pancreatic ductjejunum end-to-side continuous suture anastomosis”during clinical practices,which yields optimal clinical effect.
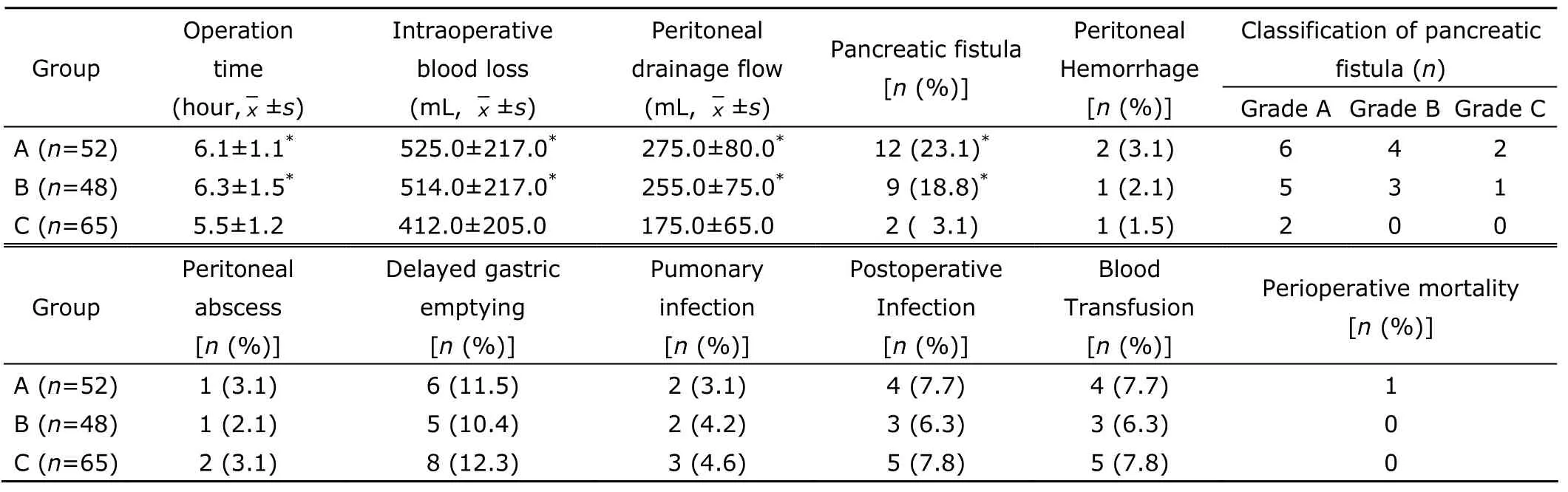
Table 3.Operation-related indexes and postoperative complications among the 3 Groups
In the present study,the novel technique called SPDJCS was applied and evaluted.The results showed that the incidence of pancreatic fistula in the group of SPDJCS(Group C) was 3.1%,significantly lower than that of Group A (23.1%) and Group B (18.8%) (P<0.05),while Groups A and B displayed no difference (P>0.05).The reason may lie in the advantages of SPDJCS∶first,the continuous suture is simple and reliable because it is free from restriction of the pancreatic duct’s size,hence no leakage;second,the suture also maintains the advantages of the conventional end-to-side mucosal anastomosis;third,the patency and fastness of anastomosis are guaranteed since the suture of pancreatic duct involves both the duct itself and the pancreatic parenchyma around it;fourth,the rate of pancreas section hemorrhage and leakage are decreased because the pancreatic section and jejunum are tightly sutured without any dead space.
In clinical practices,we recommend the following procedures when performing the SPDJCS anastomosis∶1.keep the stitch distance at 0.3-0.4 cm in continuous suture,suture as much pancreatic parenchyma as allowed,and tighten the 4-0 prolene suture after one layer is sutured;2.involve as much pancreatic duct and the surrounding pancreatic parenchyma as possible when suturing pancreatic duct,2-3 stitches are needed according to the size of the pancreatic duct.
It was also proved in this study that the operation time of Group C was much shorter than that of groups A and B,and the intraoperative blood loss and postoperative drainage amount of plasma tubes of Group C much lower(allP<0.05).The explanation may be the simplicity and convenience of SPDJCS compared with the conventional end-to-side mucosal anastomosis,therefore less demanding in operation time.There was no significant difference among the three groups in respect of other complications besides pancreatic fistula,such as peritoneal hemorrhage,peritoneal abscess,delayed gastric emptying,pulmonary infection,and postoperative infection.
According to the data of the three groups,no difference was displayed in respect of the preoperative and intraoperative status.However,in the group anastomosed with SPDJCS,the incidence of pancreatic fistula,the operation time,and the intraoperative blood loss were greatly decreased,while showing no difference in other complications.Therefore,SPDJCS may be a safe,convenient,and efficient type of anastomosis for pancreaticojejunostomy.
1.Hackert T,Werner J,Büchler MW.Postoperative pancratic fistula.Surgeon 2011;9∶211-7.
2.Whipple AO.A reminiscence∶pancreaticduodenectomy.Rev Surg 1963;20∶221-5.
3.Luo KL,Fang Z,Dong ZT,et al.Effect of modified pancreaticojejunostomy on incidence of pancreatic fistula after pancreatoduodenectomy.Chin J Gen Surg 2011;20∶909-12.
4.Lai EH,Lau SY,Lau WY.Measures to prevent pancreatic fistula after pancreatoduodenectomy∶a comprehensive review.Arch Surg 2009;44∶1074-80.
5.Cameron JL,Riall TS,Coleman J,et al.One thousand consecutive panereaticoduodenectomies.Ann Surg 2006;244∶10-5.
6.Chouman SL,He TY,Han W,et al.The effect of different drainage of pancreatic duct after pancreaticojejunostomy.Chin J Gen Surg 2011;20∶238-40.
7.Liu J.The related factors and treatment of pancreatic fistula after pancreaticoduodenectomy.Zhongguo Xiandai Shou Shu Xue Za Zhi 2011;15∶307-9.
8.Li J,Yang WP.Reconstruction of alimentary tract in pancreaticoduodenectomy.J Surg Concepts Pract 2011;16∶418-20
9.Wu W,Huang SF,Wang QW,et al.Multivariate analysis of risk factors of pancreatic fistula after pancreaticoduodenectomy.Chin J Gen Surg 2011;20∶241-4.
10.Bassi C,Dervenis C,Butturini G,et al.Postoperative pancreatic fistula∶an international study group (ISGPF)definition.Surgery 2005;138∶8-13.
11.Bassi C,Butturini G,Molinari E,et al.Pancreatic fistula rate after pancreatic resection.The importance of definitions.Dig Surg 2004;21∶54-9.
12.Ishizaki Y,Yoshimoto J,Sugo H,et al.Effect of jejunal and biliary decompression on postoperative complications and pancreatic leakage arising from pancreatojejunostomy after pancreatoduodenectomy.World J Surg 2006;30∶1985-9.
13.Dong X,Zhang B,Kang MX,et al.Analysis of pancreatic fistula according to the International Study Group on Pancreatic Fistula classification scheme for 294 patients who underwent pancreatico-duodenectomy in a single center.Pancreas 2011;40∶222-8.
14.Wang ZL,Tian BL.The prevention of pancreatic fistula after pancreaticoduodenectomy.Hua Xi Yi Xue 2011,26∶309-12.
15.Pratt WB,Maithel SK,Vanounou T,et al.Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme.Ann Surg 2007;245∶443-51.
 Chinese Medical Sciences Journal2013年1期
Chinese Medical Sciences Journal2013年1期
- Chinese Medical Sciences Journal的其它文章
- Effect of Nitric Oxide on Esophageal Cancer Cell Line TE-1
- Awareness of Cornea Donation of Registered Tissue Donors in Nanjing△
- Breast Milk Lead and Cadmium Levels in Suburban Areas of Nanjing,China
- Possible Role of Mast Cells and Neuropeptides in the Recovery Process of Dextran Sulfate Sodium-induced Colitis in Rats△
- Effect of Phenylephrine on Alveolar Fluid Clearance in Ventilator-induced Lung Injury△
- Arthroscopic Debridement and Synovium Resection for Inflammatory Hip Arthritis
