踝關(guān)節(jié)MR斷層解剖、解剖變異和病理——第二部分:解剖變異和病理(續(xù))
殷玉明
Continued from last issue Bone and cartilage disorders:
Clinically, acute ankle pain caused by ankle fracture and dislocation can be adequately evaluated with routine ankle radiographs. Some subtle fractures can be diff i cult to see on the initial radiographs even in retrospect review. Cross-sectional imaging, especially MRI is very sensitive in detecting subtle fractures.Chronic ankle pain caused by other bone abnormality including tarsal coalition, accessory navicular syndrome, Os Trigonum syndrome, osteochondral lesion of the talus, and avascular necrosis of the talus usually require MRI evaluation.
Subtle fracture of the anterior process of the calcaneus
Fracture of the anterior process of the calcaneus usually occur with forced inversion of the ankle and hind foot and usually present with vague hind foot pain. This type injury commonly causes avulsion type fracture of the anterior process of the calcaneus by increased tension of the proximal attachment of the bifurcate ligament. This type of fracture usually is very subtle and requires CT or MRI evaluation (Fig 28).
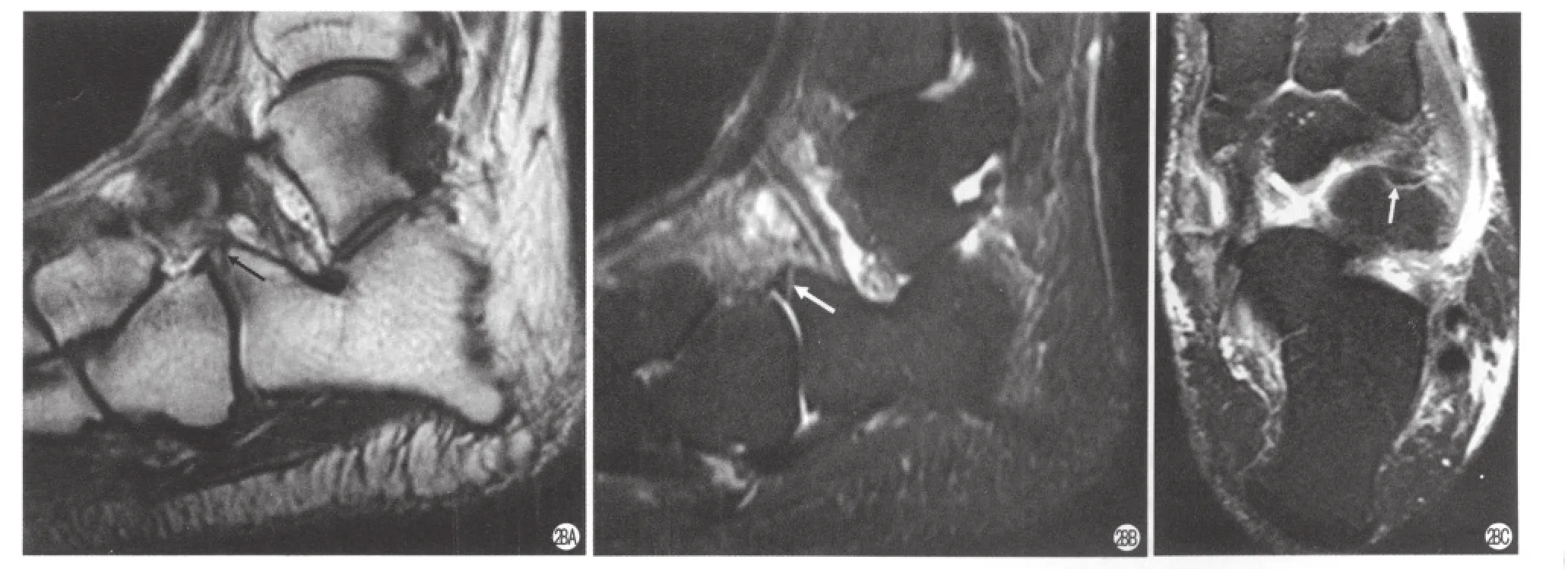
Fig 28. Subtle anterior process fracture of the calcaneus. (a)Sagittal T1 weighted image, (b)T2 weighted image with fat saturation, and (c)axial image T2 weighted image with fat saturation showed a dark fracture line in the anterior process of the calcaneus (arrow). There is no bone marrow edema adjacent to the fracture line indicating this is a previously missed subacute fracture.
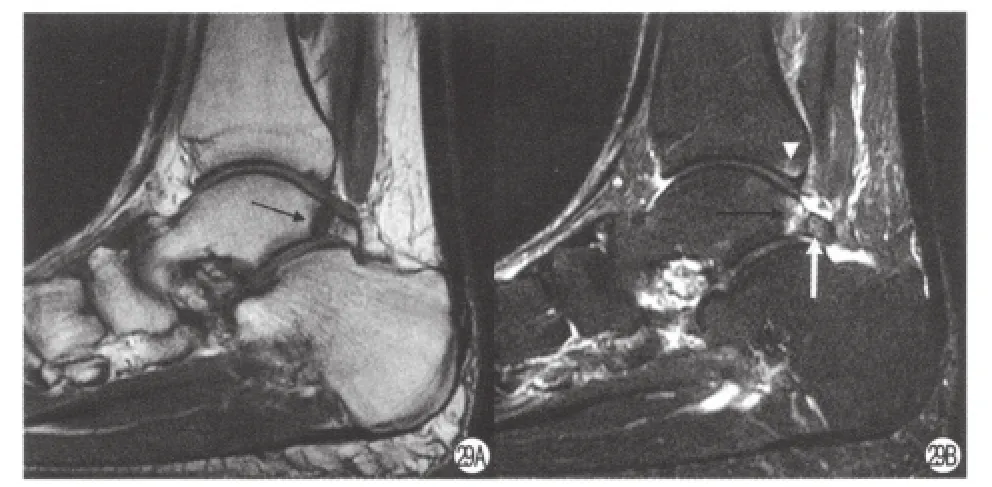
Fig 29. Os Trigonum syndrome and posterior impingement. (a)Sagittal T1 and (b)T2 weighted images with fat saturation showed reactive bone marrow edema centered at pseudoarticulation between the posterior process of the talus (black arrow)and the Os Trigonum (white arrow).Note there is focal bone marrow edema at the posterior distal aspect of the tibia (white triangle).
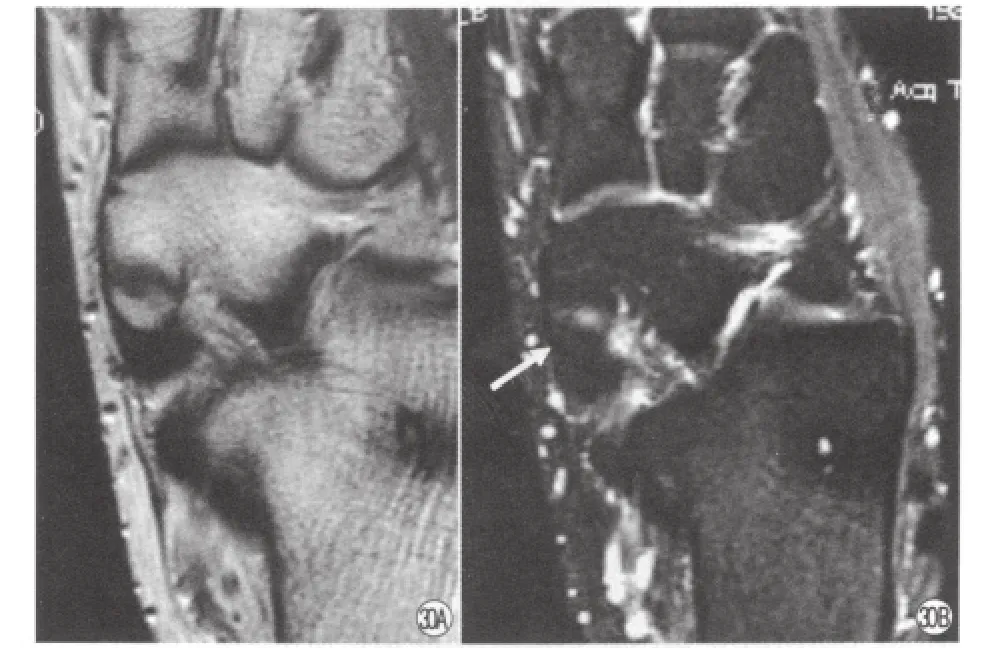
Fig 30. Asymptomatic accessory navicular. (a)Axial T1 weighted and (b)axial T2 weighted images with fat saturation showed a type II accessory navicular without bone marrow edema (arrow).
Accessory ossicles
a. Os Trigonum. There are many accessory ossicles in the region of ankle and foot. Most of them are incidental findings without causing symptom. Few of them may cause pain. One of the most commonly present ossicle located in the posterior aspect of the talus is Os trigonum. Rarely, the presents of this ossicle may cause posterior ankle pain in athlete who frequently assumes a plantar hyperflexed position. In symptomatic patient, MR imaging fi ndings demonstrate reactive bone marrow edema and cystic changes centered at pseudoarticulation between the posterior process of the talus and the Os Trigonum. There often has fluid signal between the synchondrosis and there may be associated posterior soft tissue edema due to impingement (Fig 29).
b. Accessory navicular (Os Tibiale externum, Os Naviculare Secundarium)is an accessory ossicle of the foot which is located on the medial side of foot,proximal to the medial margin of the navicular bone.Accessory navicular generally does not ossify until 9 years of age, and in about one half of cases, the accessory navicular will go on to fuse to navicular. Majority portion of posterior tibialis tendon inserted into accessory navicular bone. There are 3 types of accessory navicular.Type I, or Os tibiale externum, is a sesamoid bone within the posterior tibialis tendon near the navicular insertion.Type II accessory navicular is the ossif i cation center with residual cartilaginous synchondrosis joins the medial posterior aspect of the navicular (Fig 30). The majority or entire tibialis posterior tendon inserts on the type II accessory ossicle. The type III accessory navicular, or cornuate navicular, is a prominent navicular tuberosity.The type II accessory navicular is most commonly associated with medial ankle pain. MRI is the most specif i c imaging modality for detecting the symptomatic accessory navicular, showing edema in the bone and soft tissues (Fig 31).
Tarsal coalition
Tarsal coalition is a commonly seen congenital disorder in which an abnormal union between tarsal bones is present. The union can be osseous, fibrous,or cartilaginous. This anatomic anomaly causes abnormal articulation within the mid and hind foot which produces accelerated degenerative osteoarthritis of the hind foot and midfoot. The frequency of tarsal coalition is approximately 1%-5% in general population and 20% are bilateral. The calcaneus, talus,navicular and cuboid are commonly affected. The two most common tarsal coalitions are talocalcaneal and calcaneonavicular coalition. Several radiographic sign have been described including the “C-sign”, anterior talar beaking, narrowing of the posterior subtalar joint,and the difficult to identify the middle subtalar joint.Although the author favor CT with two-dimentional reconstruction, the CT and MRI are equally effective in demonstrating coalition. On MR imaging, normal joint space should has smooth intact articular cartilage and parallel subchondral bone. Tarsal coalition may show complete bony continuation between two tarsal bones,incomplete or partial separation of the bones, narrowing of the joint space with surface irregularity (Fig 32).
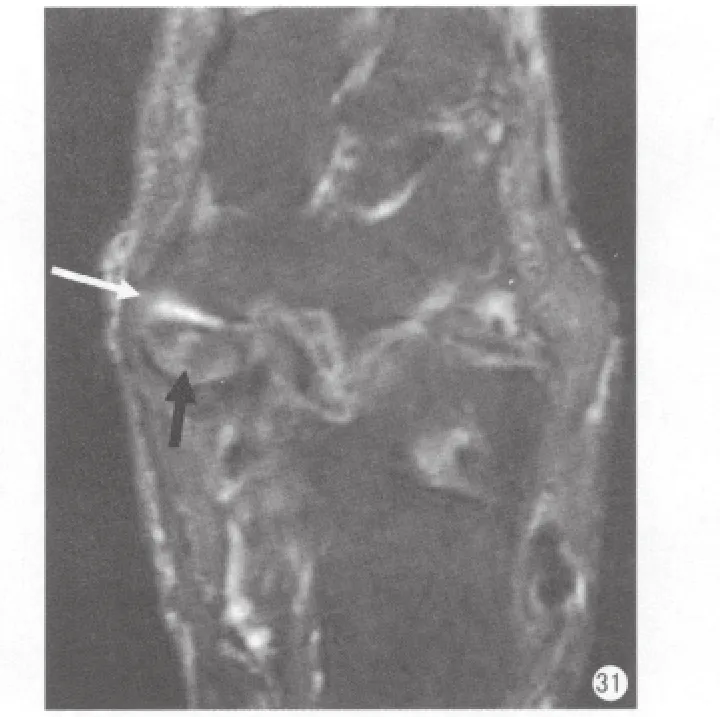
Fig 31. Accessory navicular syndrome. Axial T2 weighted image with fat saturation showed a type II accessory navicular that articulates with the navicular bone.There is bone marrow edema in the accessory navicular(black arrow)and small amount of the fluid within the pseudoarticulation (white arrow).
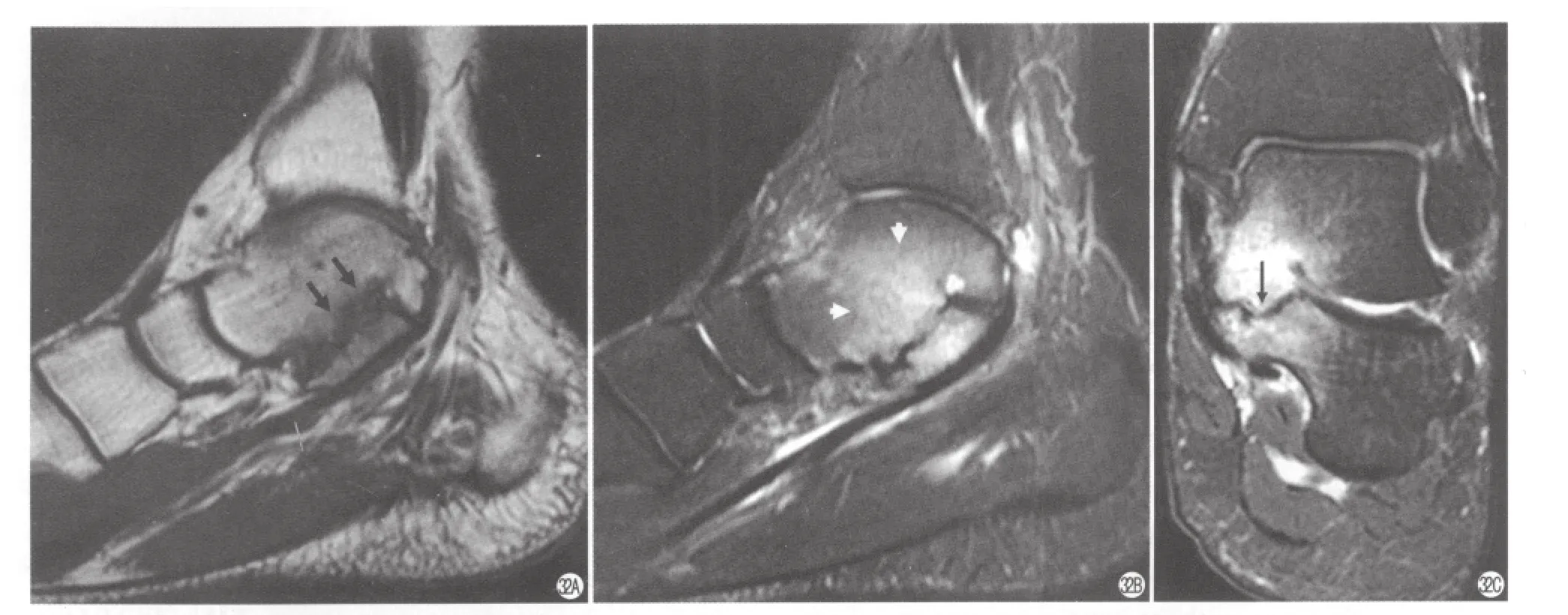
Fig 32. Talocalcaneal coalition in a 20-year-old man. (a)Sagittal T1-weighted image, (b)sagittal T2-weighted image with fat saturation and (c)coronal STIR image reveal a middle facet fibrous coalition. Note the abnormal broadening of the sustentaculum, irregularity of the articular surfaces (black arrow)and the associated bone marrow edema (short white arrows).
Osteochondral lesion of the talus (OLT)
Osteochondral lesion of the talus is the preferred term. It is also called osteochondritis dissecans,osteochondral fracture. This lesion commonly occurs in the medial or lateral talar dome. Several clinical and imaging staging classif i cations are used to describe OLTs. The more recent MR imaging classification is a more comprehensive one because it takes accounts the spectrum of MR imaging appearances of stable and unstable lesion.
MRI features include focal bone marrow edema in the talar dome starting at the subchondral region,subchondral cystic formation, subchondral fracture,articular cartilage thinning, bowing, or disruption, a detached bone fragment may form with fluid separate from the underline bone.
Stage I: subchondral trabucular fracture compression.Radiograph is normal. MRI show bone marrow edema(Fig 33).

Fig 33. Osteochondral lesion of the talus, Stage I. (a)Sagittal T1-weighted image, (b)sagittal T2-weighted image with fat saturation show focal bone marrow edema(arrow)in the subchondral bone of the talar dome.
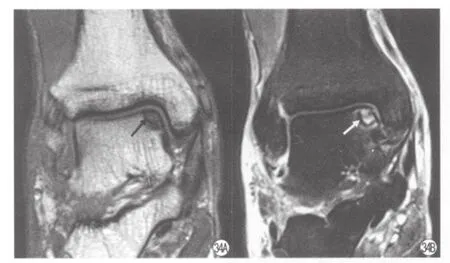
Fig 34. Osteochondral lesion of the talus, Stage II. (a)Coronal T1-weighted image and (b)coronal T2-weighted image with fat saturation showed focal bone marrow edema with subchondral cyst formation in the talar dome (arrow)and subchondral fracture at the medial talar dome.
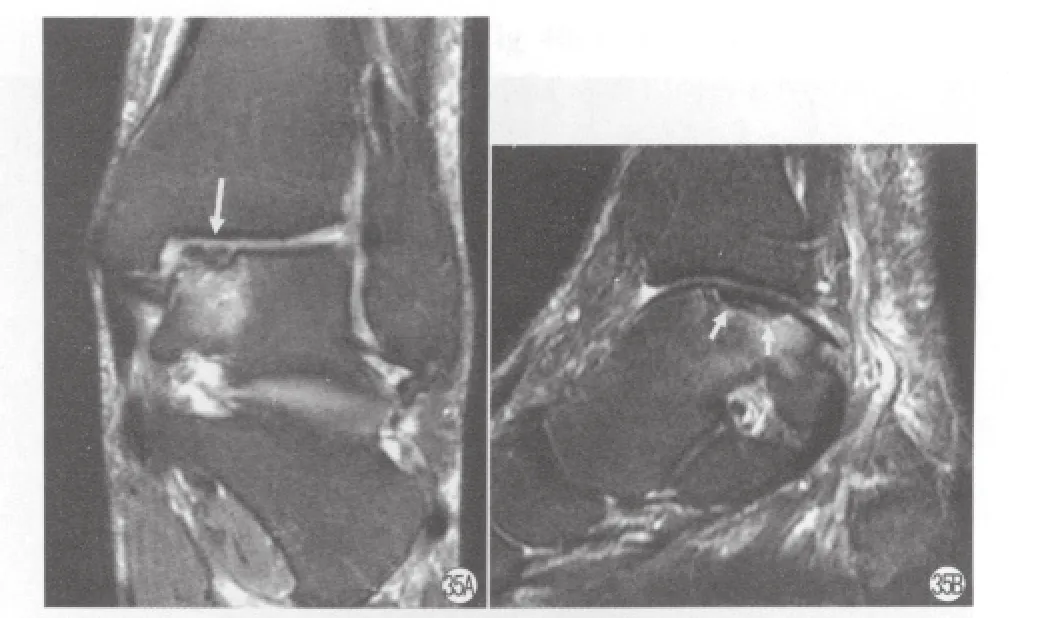
Fig 35. Osteochondral lesion of the talus, Stage III. (a)Coronal T2-weighted image with fat saturation and (b)sagittal T2-weighted image with fat saturation showed focal osteochondral fragment separated from the native bone with adjacent marrow edema in the talar dome (arrows).
Stage II: a subchondral cyst or incomplete separation of the fragment (Fig 34)
Stage III: fluid surrounds a nondetached,nondisplaced fragment (Fig 35)
Stage IV: displaced fragment
Other disorders:Sinus tarsi syndrome
The sinus tarsi is a cone shaped space between talus and calcaneus with the apex pointing to the medial side, and opening to the lateral side. It contains the cervical and interosseous talocalcaneal ligaments,the medial roots of the inferior extensor retinaculum,neurovascular structures, and fat. Patients with sinus tarsi syndrome present with hindfoot instability and pain along the lateral aspect of the foot. Although it is a clinical diagnosis, MR imaging is the only non-invasive method to detect this abnormality.
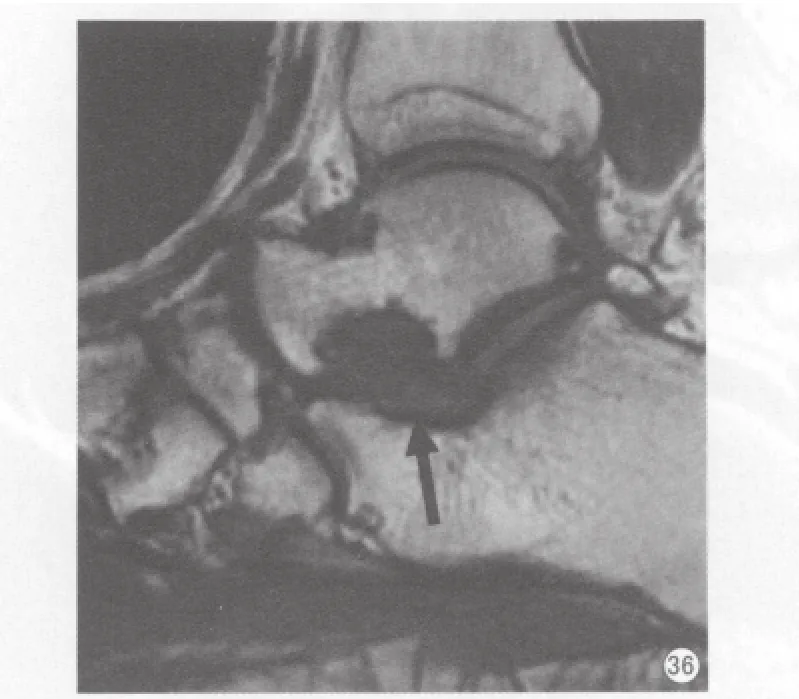
Fig 36. Sinus tarsi Syndrome. Sagittal T1-weighted image showed loss of the fat signal within the sinus tarsi (arrow).
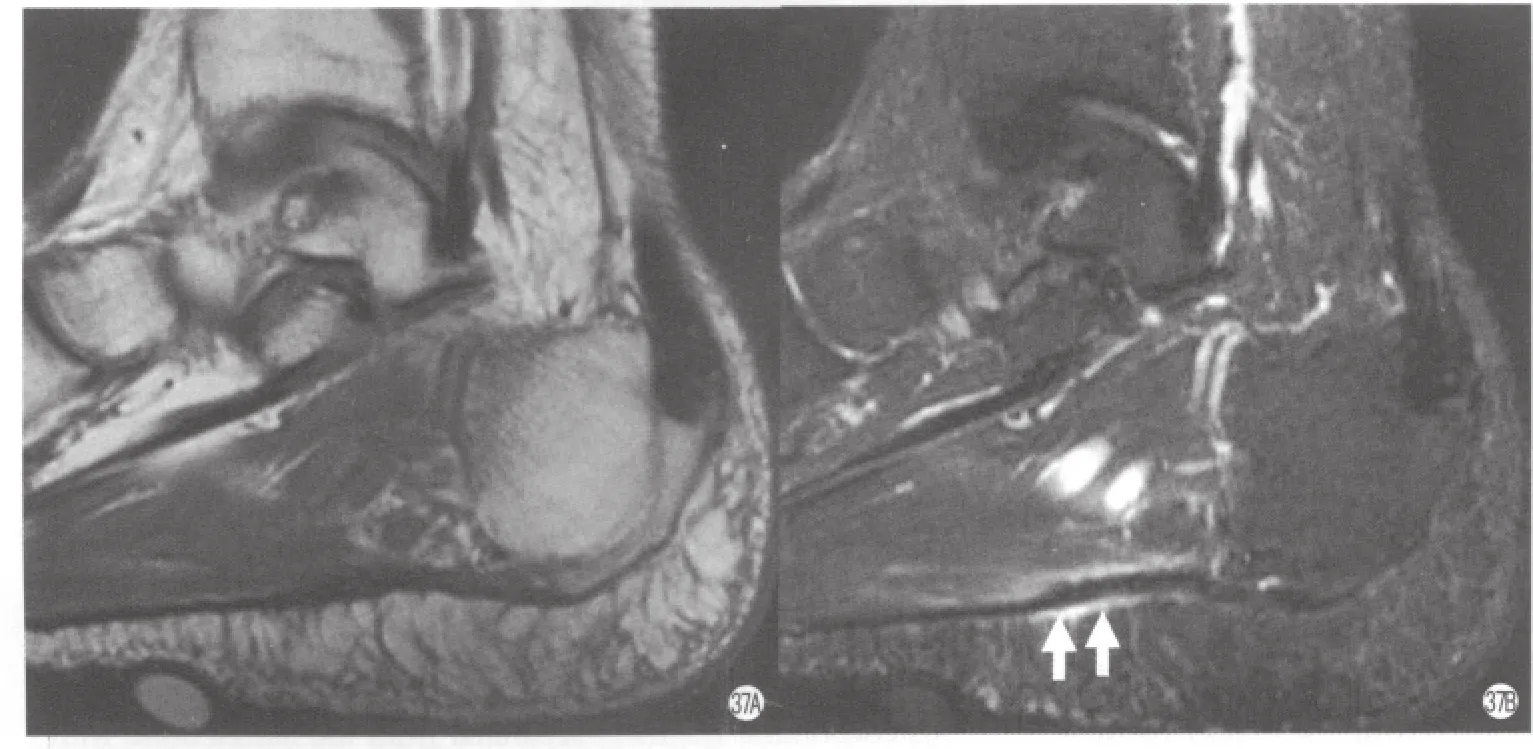
Fig 37. Mild plantar fasciitis in a 31 years old patient. (a)Sagittal T1, (b)sagittal T2 weighted with fat saturated images, and (c)coronal T2 weighted with fat saturated images showed mild thickening of the proximal plantar fascia near the origin with increased sign (arrow).Note there is mild surrounding soft tissue edema in the region of the fasciitis.
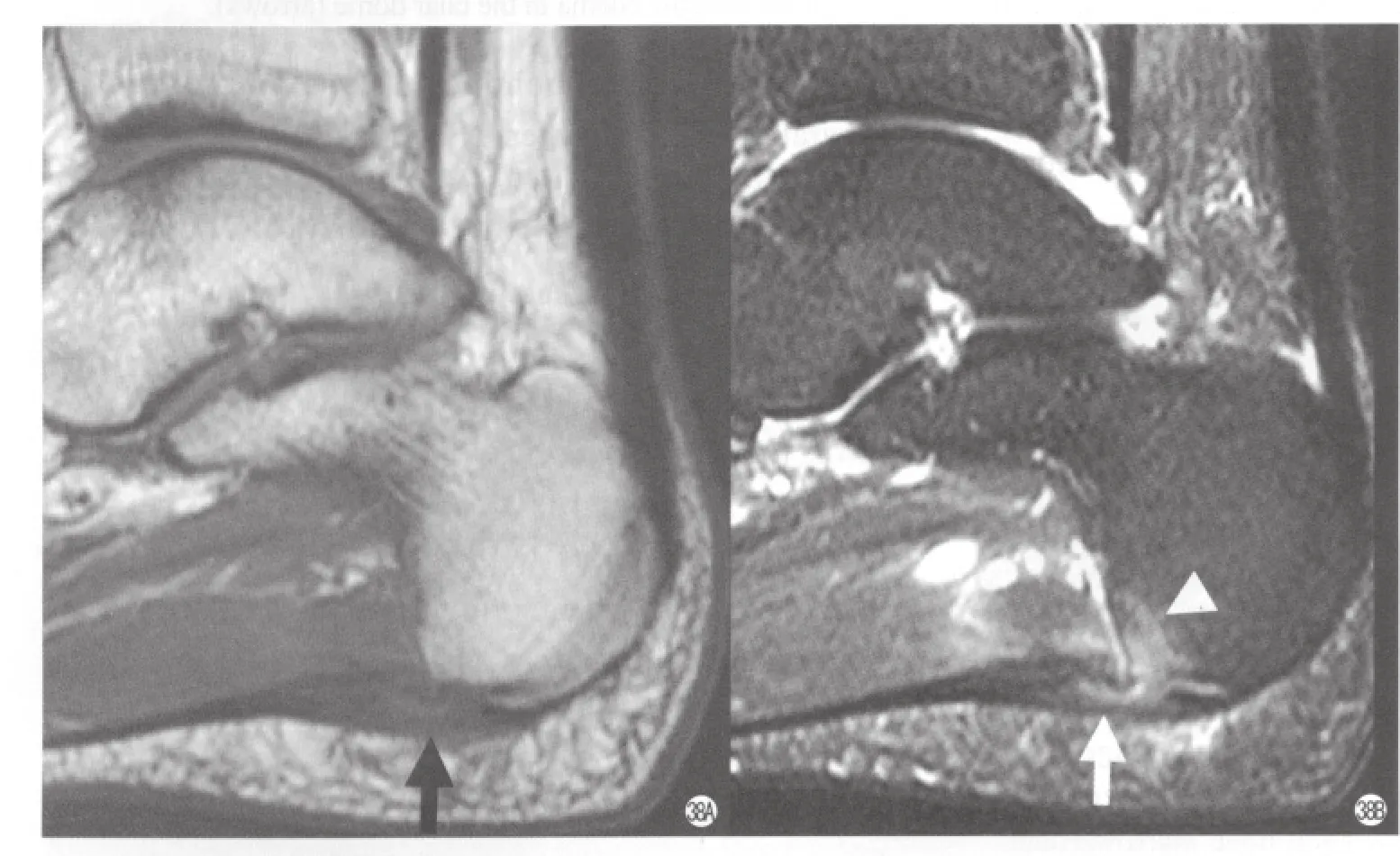
Fig 38. Moderate plantar fasciitis in a 33 years old patient. (a)Sagittal T1, (b)sagittal T2 weighted with fat saturated images showed moderate thickening of the proximal plantar fascia near the origin with increased sign (arrow). Note there is focal bone marrow edema at the calcaneus tubercle near the plantar fascia insertion (arrowhead). There is surrounding soft tissue edema in the region of the fasciitis.

Fig 39. Severe plantar fasciitis in a 36 years old patient with complete tear. (a)Sagittal T1 and (b)T2 weighted image with fat saturation showed thickening of the proximal plantar fascia near the origin with increased sign. Note there is fl uid signal in the proximal origin of the Achilles tendon between the tendon and the bone (arrow).
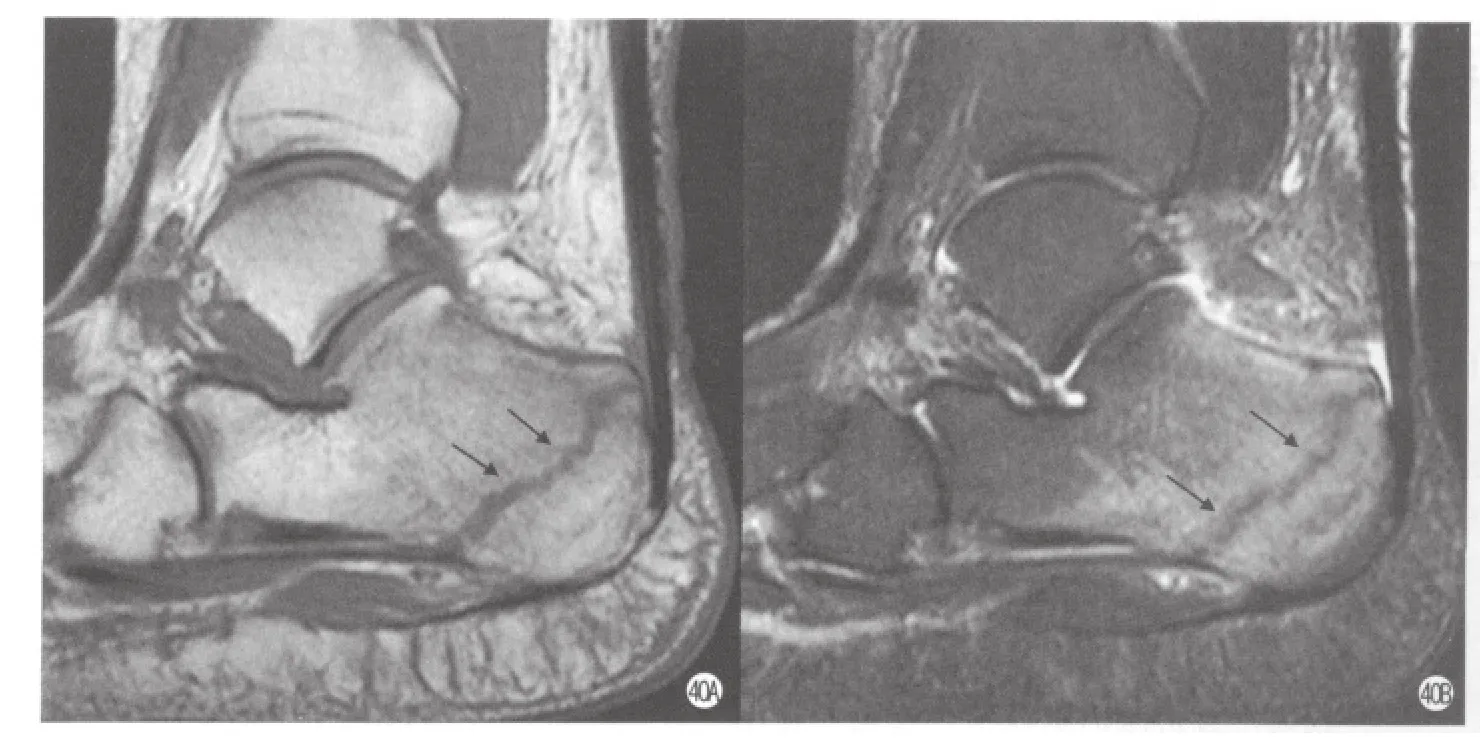
Fig 40. Calcaneus stress fracture.(a)Sagittal T1 and (b)T2 weighted image with fat saturation showed a line dark signal through the posterior calcaneus on both T1 and T2 weighted images with adjacent bone marrow edema (arrow).
The MR imaging characteristics of sinus tarsi syndrome include the obliteration of fat in the sinus tarsi space (Fig 36). The space itself is replaced by either fluid or scar tissue, and the ligaments may be disrupted. Osteoarthritis of the subtalar joint and subchondral cysts may be present in advanced cases.Normal recesses from the posterior subtalar joint may frequently extend into the sinus tarsi and should not be misinterpreted as pathologic conditions.
Plantar fasciitis
Plantar fasciitis is a degenerative change of the plantar fascia. Commonly present with heel pain. This disorder usually occurs near the origin of the plantar fascia. MR imaging is the only way to be able to see non-invasively. On MR images showed thickening of the plantar fascia with increased signal and edema of the peritendinous soft tissue (Fig 37). Sometime, it associated with partial tear (Fig 38)or complete tear (Fig 39).
Stress fracture
Fatigue-type stress fracture of the ankle and hindfoot are commonly occurs in athletes, especially in distance runners or sports participants who substantially increase or change their training routine and in those returning from injury. This type of fracture can be subtle initially on radiograph. This type fracture sometimes can be appreciated on radiology as a transverse linear increased density perpendicular to the long axis of bones such as distal tibial metaphysis, talar neck, posterior calcaneal body, and navicular body. MR images show hyposignal intensity on T1 weighted images and hypersignal intensity on T2 both weighted images with a linear dark signal on both T1 and T2 weighted images. This linear dark signal is the fracture line with bone marrow edema centered at this line (Fig 40).
Summary
MR imaging is a very valuable in the diagnosis and differential diagnosis of ankle disorder. When a bone abnormality is suspected, the routine ankle should be obtained fi rst. Then the MRI should be the next step for further evaluation of the ankle.
Acknowledgement
The author would like to thank professor Shinong Pan (潘詩農(nóng))for his excellent translation of the abstract from English to Chinese.

