Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
Xiao-Hua Pan, Yu-Fei Tao, Ming-Min Yang, Xiao-Li Shen, Jiao Si, Ming Li, Ning Fan
Shenzhen Eye Hospital, Jinan University, Shenzhen 518040,Guangdong Province, China
Dear Editor,
Iridocorneal endothelial syndrome (ICE) is a rare ocular disease first proposed by Eagleet al[1]in 1979.It is mainly characterized by corneal endothelial abnormalities,accompanied by iris atrophy, iris pigmented nodules and peripheral anterior synechiae.ICE syndrome is typically unilateral, and classified into three clinical variants based on the changes of the cornea and iris, including progressive iris atrophy, Chandler’s syndrome, and Cogan-Reese syndrome.Chandler’s syndrome mainly involves corneal changes such as corneal edema, bullous keratopathy and corneal endothelial decompensation, accompanied by mild iris atrophy[2].This article reports a rare case of bilateral ICE syndrome.The written informed consent was obtained from the patient, and this study was in accordance with the Declaration of Helsinki.
CASE REPORT
A 58-year-old woman complaining of a sudden decrease in vision, accompanied by pain and redness bilaterally for 3d, was referred to Shenzhen Eye Hospital in 2019.Her symptoms did not relief after the use of timolol, brinzolamide and pilocarpine eyedrops with the diagnosis of acute angle-closure glaucoma at another hospital.She had undergone laser peripheral iridotomy for both eyes due to narrow angles in 2009 and did not present with iris abnormalities.Over the past year, she had experienced recurrent eye redness, which relieved after using antibiotic eye drops by herself.She denied any family history, trauma or systemic diseases.At the first examination, the best-corrected visual acuity(BCVA) was 20/200 in right eye and 20/100 in left eye.The intraocular pressure (IOP) was 50 and 45 mm Hg respectively.The results of slit lamp and complementary examination of the patient were shown in Figure 1.Considering the high IOP, we adjusted the medications to timolol, brinzolamide,brimonidine tartrate, travoprost, tobramycin dexamethasone eye drops, methazolamide tablets and mannitol drip.Her vision improved to 20/25 and 20/22 and her IOP decreased to 25 and 20 mm Hg respectively.The central cornea became transparent so that further examinations were carried out for a definite diagnosis (Figure 1).The gonioscopy showed angle-closure and 360 degrees of high-positioned peripheral iris synechiae.The ultrasound examination and fundus photography after IOP dropping showed the posterior segment of the eye was generally normal without obvious signs of inflammation and ischemia.The corneal endothelial microscopy and confocal microscopy revealed decreased,enlarged, irregular endothelial cells with activated nuclei and a few owl eye cells instead of ICE cells.Therefore, the patient was diagnosed of secondary angle-closure glaucoma.Trabeculectomy surgery was performed bilaterally because the IOP could not be controlled by anti-glaucoma eyedrops.The aqueous humor was taken during the operation process and the aqueous humor test results showed inconspicuous elevation of antibodies and negative results of nucleic acid for cytomegalovirus, herpes simplex virus (HSV), varicella-zoster virus or Epstein-Barr virus.
In 2022, the patient returned for a follow-up examination without any eye redness or pain, with the IOP kept under 18 mm Hg bilaterally in the past three years.BCVA was 20/20 and 20/25, the IOP was 16 and 17 mm Hg for the right and left eye separately.As shown in Figure 2, the edema of peripheral cornea became worse both in range and in severity without any keratic precipitates (KPs).Corneal endothelial microscopy showed increased corneal thickness and cell size,decreased cell density and hexagonal cell ratio in both eyes compared to how they were three years ago.Cornea confocal microscopy showed an increase in nuclear activation and spotlike holes, and a decrease in owl eye cells[3].All the changes mentioned above suggest the aggravating corneal endothelium cells damage even under IOP control, so the patient was diagnosed of bilateral Chandler’s syndrome.
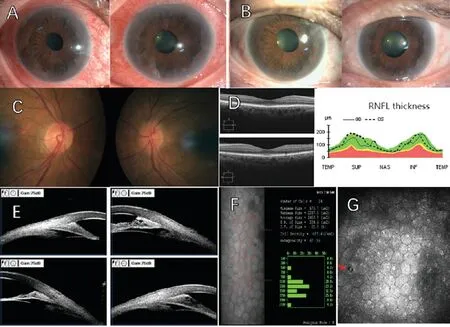
Figure 1 The ophthalmic examination of the patient’s first visit in 2019 A: Diffuse congestion of the conjunctiva, epithelial and stromal edema of the cornea with a sudden increased IOP in both eyes.B: The conjunctiva congestion reduced, the central cornea regained transparency, but the peripheral cornea remained hydropic because of 360 degrees peripheral anterior synechiae and impaired corneal endothelial function after IOP dropping.Several pigmented KPs were seen without specular reflected light called “hammered silver” appearance in corneal endothelial cells using the slit lamp.The anterior chamber flare was negative.C: Sharp optic disc margins in right eye and blurred in lefteye.D: The OCT scanning showed that the macula and RNFL thickness were generally normal.E: High-positioned peripheral iris adhesions to the cornea and stroma separation under UBM.F: Corneal endothelial microscopy revealed decreased and enlarged endothelial cells without ICE cells.G: Corneal confocal microscopy showed enlarged corneal endothelial cells, reduced hexagonal structures, nuclear activation, several highly reflective KPs and scattered owl eye cells.The red arrow showed a owl eye cell, which had high internal reflection with a surrounding low-echo band.IOP: Intraocular pressure; KPs: Keratic precipitates; OCT: Optical coherence tomography; RNFL: Retinal nerve fiber layer; UBM: Ultrasound biomicroscopy; ICE: Iridocorneal endothelial syndrome.
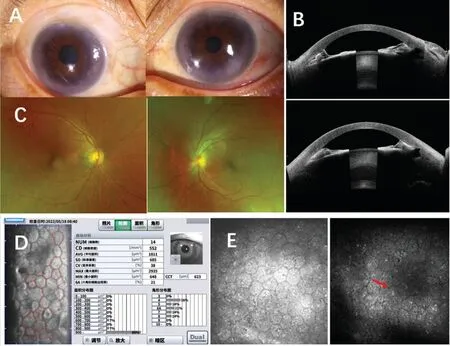
Figure 2 The ophthalmic examination of the patient three-year follow-up in 2022 A: The cornea was transparent in the center and cloudy in the periphery because of peripheral anterior synechiae and impaired corneal endothelial function.Neither KPs nor “hammered silver”appearance was seen because of cornea edema.B: High-positioned peripheral iris adhesions to the cornea under ASOCT.C: Normal optic disc,macula and retina of the posterior pole.D: Corneal endothelial microscopy showed increased corneal thickness, irregular endothelial cells of different sizes, decreased hexagonal cells and cell density, increased cell area and coefficient of variation.E: Corneal confocal microscopy showed endothelial cells were significantly enlarged with reduced hexagonal, much nuclear activation and spot-like holes (the red arrow) and very few owl eye cells.KPs: Keratic precipitates; ASOCT: Anterior segment optical coherence tomography.
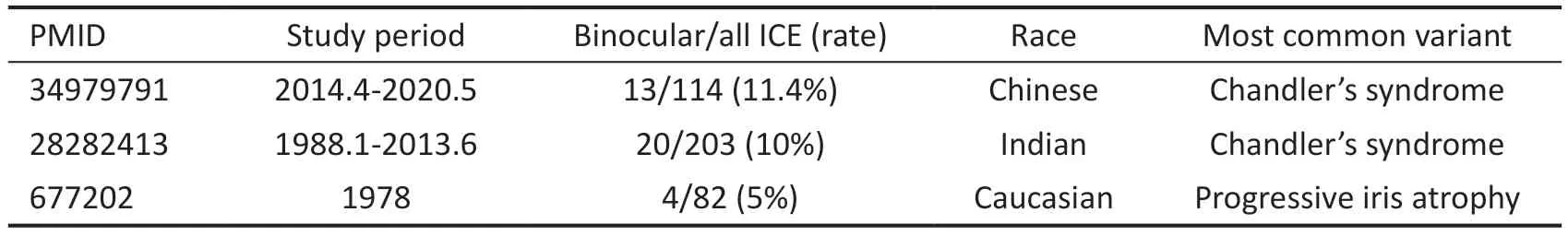
Table 1 Large sample studies of binocular ICE syndrome
DISCUSSION
The ICE syndrome is rare with a concealed onset.In other words, patients often present with severe vision-threatening conditions such as corneal endothelial decompensation or glaucoma.In terms of epidemiological features, ICE syndrome is typically unilateral with extremely few bilateral cases occasionally reported.Currently, studies of binocular ICE syndrome were dominated by case reports[4-6].Large sample studies of binocular ICE syndrome were rare and mainly concentrated in Asia (Table 1)[7-9].
It can be difficult to distinguish ICE syndrome from recurrent viral anterior uveitis, posterior polymorphous corneal dystrophy(PPCD) and Axenfeld-Rieger syndrome, when the clinical manifestations of ICE syndrome are atypical.At the patient’s first visit with acute IOP elevation, we diagnosed secondary angle-closure glaucoma and couldn’t identify Chandlers syndrome or recurrent viral uveitis.Three years after trabeculectomy, the IOP was controlled without recurring inflammation.However, the corneal edema persistently worsened.Combination of corneal endothelial microscopy and confocal microscopy led to the clarification of Chandlers syndrome instead of viral anterior uveitis.The KPs might be considered to result from iris atrophy and depigmentation due to acute IOP elevation.PPCD is a corneal endothelial disorder usually with family members diagnosed with PPCD.This disease is notable on confocal corneal microscopy for the irregular hyperreflective thickening of Descemet’s membrane,the cratered, grooved or ridged hypo-reflective dark zones of corneal endothelial layer, which the patient’s symptoms did not match.Axenfeld-Rieger syndrome often onset in juvenile with family history.Typical sign includes posterior corneal embryonic ring and pupil abnormalities in both eyes with facial, dental, and umbilical defects, which did not conform with the patient’s symptoms[2].
The main pathological changes of ICE syndrome concentrate in the corneal endothelial cells.To date, there are three kinds of theories for the pathogenesis of ICE syndrome: 1) Campell membrane theory: a membrane formed from abnormally proliferating and variant corneal endothelial cells extended to the iridocorneal angle in ICE syndrome.2) Inflammatory and viral infection theory: studies suggested that virus was associated with the pathogenesis of ICE syndrome.3) Vascular theory: iris vascular had functional disorder in ICE syndrome but lacking substantial evidence[2].
In this case, the follow-up examination after three years showed a decrease in owl eye cells and an increase in spot-like holes.The presence of owl eye cells can effectively suggest corneal endotheliitis of cytomegalovirus.However, a patient diagnosed as corneal endotheliitis of HSV infection would also present owl eye cells[10].The spot-like holes refer to the dark round holes in the corneal endothelial layer, whose diameter is equal to that of one endothelial cell.So it is speculated that the formation of spot-like holes may result from the shedding of individual endothelial cells.Some researchers believe that the spot-like holes are characteristic manifestation of HSVinfected corneal endotheliitis.Therefore, the owl eye cells and spot-like holes both support the infection of virus precisely the HSV.All evidences above support the theory of inflammatory and viral infection of ICE syndrome.
In conclusion, our article reported a rare case of bilateral ICE syndrome with complete clinic examinations and long-time follow-up.Three years after the surgery, the diagnosis and the theory of inflammatory and viral infection of ICE syndrome were supported by the findings of corneal endothelial microscopy, corneal confocal microscopy and aqueous humor analysis.
ACKNOWLEDGEMENTS
Authors’ contributions:Pan XH and Tao YF drafted the manuscript, Yang MM edited the photos, Shen XL and Si J collected the patient information, Li M analyzed and interpreted the result of corneal confocal microscopy, Fan N critically revised the manuscript and supervised the project.All
authors read and approved the final manuscript.
Foundations:Supported by the National Natural Science Foundation of China (No.82271087); Science and Technology Innovation Committee of Shenzhen (No.JCYJ20190807153005579); Shenzhen Science and Technology Program (KCXFZ20230731093359004).
Conflicts of Interest: Pan XH,None;Tao YF,None;Yang MM,None;Shen XL,None;Si J,None;Li M,None;Fan N,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
- On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
- Mesenchymal stem cells for repairing glaucomatous optic nerve
