Surgical management of gallstone ileus after one anastomosis gastric bypass: A case report
Elie El Feghali, Rhea Akel, Bilal Chamaa, Daniel Kazan, Ghassan Chakhtoura
Abstract
Key Words: Gallstone ileus; One anastomosis gastric bypass; Bariatric surgery; Ⅰntestinal occlusion; Bilio-digestive fistula; Enterolithotomy; Case report
INTRODUCTION
One anastomosis gastric bypass (OAGB) or mini bypass was first performed by Dr. Robert Rutledge in 1997[1]. It is both a restrictive and malabsorptive bariatric surgical procedure for the treatment of morbid obesity. It was developed as a faster and simpler alternative to the Roux en Y gastric bypass and is the fourth most performed bariatric technique in Europe and in Asia[2]. It is an effective surgical technique in terms of both weight loss and the resolution of comorbidities[3]. Nevertheless, like any other surgical procedure, OAGB can be associated with potential complications such as anastomotic leaks in 0.5 to 5.0 percent of cases, bleeding 0.2 to 2.0 per cent, nutritional deficiencies 5 to 50 per cent[4]. In addition, intestinal obstruction or occlusion is a possible complication after the OAGB with an incidence of 1 to 10 per cent[5] causing symptoms such as abdominal pain, nausea and vomiting and constipation. The most common etiologies of intestinal occlusion post-OAGB include internal hernias, adhesions, strictures and bowel kinking and/or twisting. In our case report, we are going to be present a rare cause of intestinal occlusion post-OAGB, the gallstone ileus (GI).
CASE PRESENTATION
Chief complaints
A 66-year-old female presented to the ER for abdominal pain and vomitting.
History of present illness
She had a 4-d history of food intolerance with post-prandial vomiting and diffuse colic type abdominal pain, her bowel movements were maintained. She denied having previously experienced similar symptoms or symptoms suggesting of cholecystitis during her post-operative interval.
History of past illness
She is known to have bipolar disease treated with Perphrenazine 8 mg and known to be a 5 pack/year smoker. She was operated of OAGB 6 years ago for morbid obesity [body mass index (BMI): 66.7 kg/m2]. Previous comorbidities that included hypertension and diabetes mellitus were rectified after her weight loss of 90 Kg (BMI: 26.66 kg/m2). Previous surgical interventions include 2 C-section deliveries.
Personal and family history
She has no significant family history.
Physical examination
On physical examination, her abdomen was soft with mild tenderness in the lower right quadrant. She had a supraumbilical hernia from her previous intervention.
Laboratory examinations
Her labs showed a mild hyper-leukocytosis white blood cell 12000 and C-reactive protein level was 80.8, her liver enzymes were in the normal range.
Imaging examinations
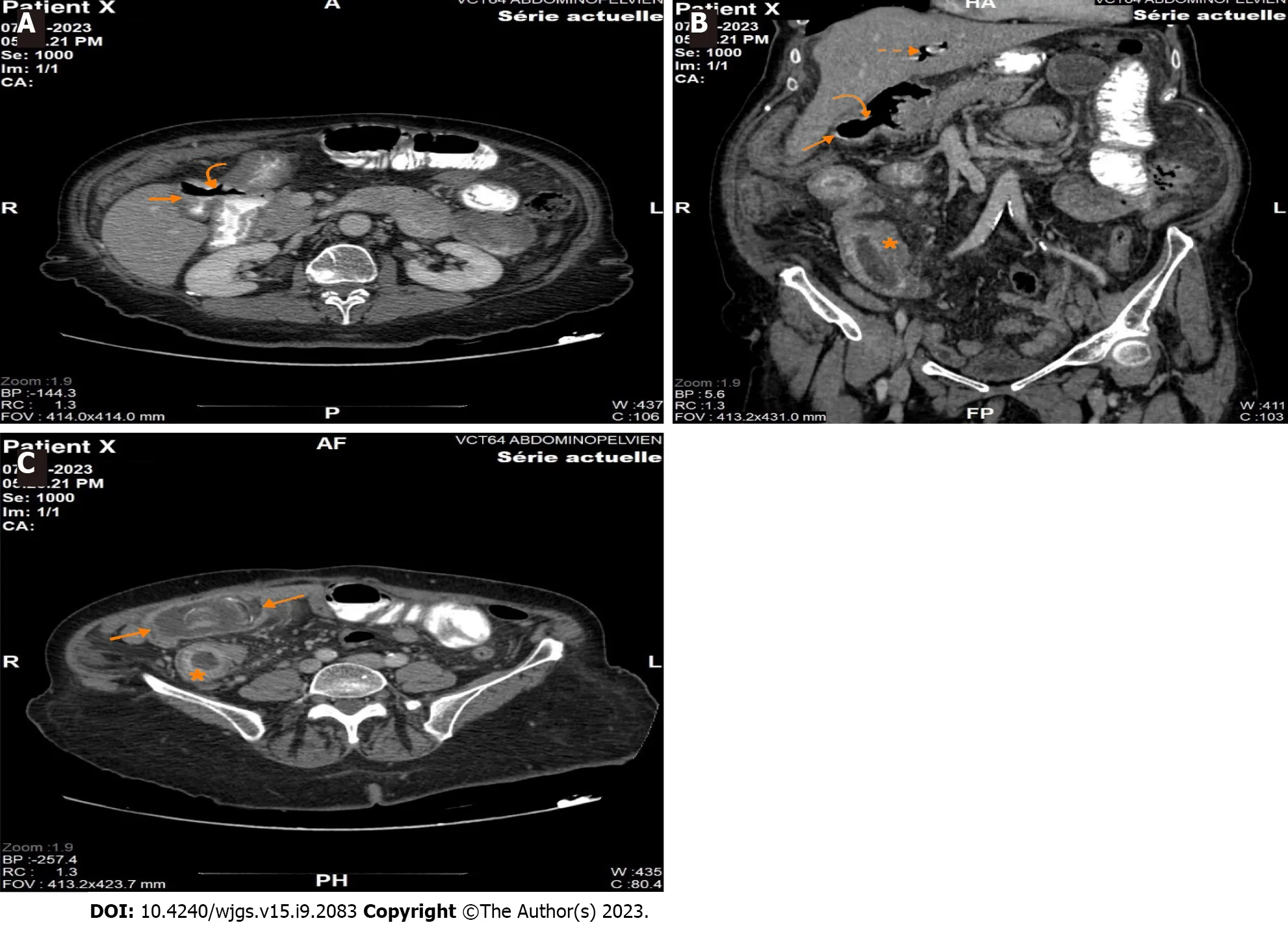
Figure 1 Computed tomography scan. A: Axial section of contrast-enhanced computed tomography (CT) shows a gallbladder containing a hydro-aeric level with passage of ingested contrast medium (straight arrow) associated to a visible communication of 15 mm between the gallbladder and the duodenal bulb (curved arrow); B: Coronal reconstructed image (using multiplanar reconstruction) of contrast-enhanced CT shows the defect between the gallbladder and the duodenal bulb(curved arrow), the gallbladder filled with air (straight arrow) as well as pneumobilia within the intrahepatic biliary ducts (dotted straight arrow). Note that the distal ileum is mildly dilated, markedly thickened with increased mucosal enhancement (asterisks); C: Axial section of contrast-enhanced CT shows a gallstone measuring almost 45 mm (two arrows) impacted in the distal ileum, with marked thickening and increased mucosal enhancement within the upstream ileum (asterisks).
An abdomino-pelvic computed tomography scan with injection and ingestion of contrast was ordered (Figure 1). It showed a fistulous tract between the gallbladder and the duodenal bulb, extending over 15 mm. The fistula was confirmed with the leakage of the ingested contrast in the lumen of the gallbladder, which was not distended and contained an air-fluid level. It was associated with pneumobilia and small bowel dilation of 42 mm in diameter, with an intestinal segment in the right lower quadrant showing parietal thickening and submucosal edema upstream of a transition zone located at the level of the right iliac fossa, downstream of a probable oval intraluminal calculus of 45 mm. The previous findings evoking a GI with a probable gallstone located at the level of the efferent alimentary loop. It is associated with a trabeculation of the fat at the level of the two flanks, especially on the right, with perihepatic and pelvic ascites of low abundance. Sequelae of gastric surgery with gastro-jejunal anastomosis (Roux en Omega) was identified.
FINAL DIAGNOSIS
She was thus admitted for adequate treatment of her GI.
TREATMENT
After establishing the diagnosis of GI and acquiring the written consent of the patient, she was transferred to the operating room for a diagnostic laparoscopy and subsequent enterolithotomy. A nasogastric tube was inserted and she was adequately hydrated.
Open coelioscopy was performed and a 10 mm port was introduced. Pneumoperitoneum was created with a PCO2 of 12 mmHg. Two para-umbilical 5 mm ports were introduced under vision. There were multiple adhesions over the previous gastro-jejunal anastomosis and over the gallblader. The entero-biliary fistulae were not visualized, even after adhesyolysis. The afferent biliopancreatic loop was normal in diameter whereas the efferent alimentary loop was distended. The small bowel was run downwards until the obstructed ileal loop was identified. A 5 cm para-umbilical midline incision was made and the bowel segment was exteriorized. A horizontal enterotomy was performed to allow the extraction of an ovoid shaped yellow-brown stone measuring 5 cm × 3 cm × 1 cm approximately (Figure 2). The enterotomy was closed transversely with a double layer of absorbable sutures, and the small bowel was returned to the abdomen. The incision was approximated with non-absorbable monofilament sutures.
OUTCOME AND FOLLOW-UP
The patient’s recovery was uneventful with return of bowel function on postoperative day two and diet advanced as tolerated. The patient was discharged home in improved condition on postoperative day four.
DISCUSSION
Rapid weight loss after bariatric surgery is associated with an increase in cholelithiasis, especially when the weight loss is greater than 25 per cent of the preoperative weight[6] with 38 per cent of patients developing gallstones within 6 mo, of which, 41 per cent will ultimately develop symptomatic cholelithiasis[7].
Gallstone ileus or Bouveret’s Syndrome is a rare but serious complication of cholelithiasis as it occurs in 0.3 per cent of patients[8,9]. It results when a supracentimetric gallstone, which was formed during a medically treated or neglected cholecystitis, migrates from the gallbladder to the bowel through a biliary enteric fistula, the most common being a cholecystoduodenal fistula, and causes an obstruction, in more than 70% of cases at the level of the terminal ileum[10].
GI is considered to be implicated in 1 to 4 per cent of mechanical bowel obstruction, and accounts for a quarter of nonstrangulated small bowel obstruction in patients above the age of 65 years, with a mortality rate between 15 to 18 per cent[9] with a female to male ratio of 3.5-6.1[11].
The diagnosis of GI is both clinical and radiological. GI has nonspecific symptoms such as nausea and/or vomiting associated with abdominal pain, bloating and constipation. The abdominal computed-tomography scan is the gold standard to establish the diagnosis. Rigler’s triad of pneumobilia with small bowel obstruction caused by an ectopic gallstone within the bowel is observed in 40 to 50 per cent of cases[12].
Conservative measures such as nil per os status, nasogastric tube decompression with adequate intravenous hydration may be sufficient in select clinically stable patients with partial bowel obstruction and stones < 2 cm in size[8]. However, GI often requires urgent surgical management, laparoscopically in 10% of cases[13], which allows delineation of the anatomy with decreased bowel manipulation and subsequent safe stone extraction and reduced risk of intestinal content spillage.
The choice of surgical intervention is a subject of controversy[14]. A one or two stage procedure may be proposed: either enterolithotomy alone or enterolithotomy with cholecystectomy and eventual repair of the biliary fistula[15]. Nevertheless, the one stage approach is discouraged in view of the significant mortality (16.9%) compared with the two staged procedure (11.7%)[9]. In addition, laparoscopically assisted enterolithotomy has been credited with a favorable impact as it can be recommended for both diagnosis and treatment[16]. Prevention of symptomatic cholelithiasis after gastric bypass could be achieved by either prophylactic cholecystectomy or administration of ursodiol. In the one hand, prophylactic cholecystectomy during gastric bypass is a debatable subject. Its supporters argue that it is safe and would prevent both the morbidity associated with symptomatic cholelithiasis and a subsequent operation. Those who oppose to it cite that the safety of secondary cholecystectomy with an increase in operative time and length of stay do not justify the prophylactic cholecystectomy[17]. In the other hand, administration of a daily dose of 600 mg of ursodiol after gastric bypass was associated with a significant reduction in the incidence of cholelithiasis compared with placebo at 6 mo (2%vs32%)[18].
To our knowledge, this is the first documented report of GI in a patient after OAGB. The GI diagnosis was established after correlation of the clinical and radiological findings of the patient. The fact that the patient presented to the emergency department with small bowel obstruction symptoms and the CT-scan confirmed the GI diagnosis with the presence of Rigler’s triad previously discussed. The decision was to perform a two-staged procedure. Laparoscopically assisted enterolithotomy was preformed because it is in our opinion the safest and fastest therapeutic modality. At our institution, our current practice is to perform the OAGB without prophylactic cholecystectomy given that, if needed, a laparoscopic cholecystectomy is feasible in the case of a symptomatic cholelithiasis.
CONCLUSION
In conclusion, the incidence of cholelithiasis significantly increases after bariatric surgery and may lead to serious complications such as gallstone ileus, which require further operations.
FOOTNOTES
Author contributions:El Feghali E wrote the manuscript; Akel R provided the radiology images and their respective annotations; Chamaa B and Kazan D performed the research; Chakhtoura G designed the research study; and all authors have read and approve the final manuscript.
Informed consent statement:Informed written consent was obtained from the patients for the publication of this report and any accompanying images.
Conflict-of-interest statement:There are no conflict-of-interest to disclose.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Lebanon
ORCID number:Elie El Feghali 0009-0004-0075-1792.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
 World Journal of Gastrointestinal Surgery2023年9期
World Journal of Gastrointestinal Surgery2023年9期
- World Journal of Gastrointestinal Surgery的其它文章
- Quantitative evaluation of colorectal tumour vasculature using contrast-enhanced ultrasound: Correlation with angiogenesis and prognostic significance
- Risk factors for myocardial injury during living donor liver transplantation in pediatric patients with biliary atresia
- Value of enhanced computed tomography in differentiating small mesenchymal tumours of the gastrointestinal from smooth muscle tumours
- Multifactor analysis of the technique in total laparoscopic gastric cancer
- Clinical significance of serum oxidative stress and serum uric acid levels before surgery for hepatitis Brelated liver cancer
- Prediction model of stress ulcer after laparoscopic surgery for colorectal cancer established by machine learning algorithm
