Successful treatment of a patient with diff use alveolar hemorrhage and anti-neutrophil cytoplasmic antibody-associated vasculitis
Yao Liu, Qiu-ling Zhang, Heng-jun Liu, Wei Wang, Yi Zhou, Peng Xu
Emergency Department of Drum Tower Hospital, the Affi liated Hospital of Nanjing University Medical School, Nanjing 210008, China
Dear editor,
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a cluster of disorders characterized by inflammation and destruction of smalland medium-size blood vessels as well as the presence of circulating ANCA with the major target antigens identified as proteinase 3 (PR3) and myeloperoxidase (MPO).The lungs are frequently involved in systemic vasculitis, where diff use alveolar hemorrhage (DAH) complicated with acute respiratory failure is one of the most serious symptoms and usually results in unacceptably high mortality.
The clinical features of DAH include hemoptysis,severe anemia, and progressive acute respiratory distress syndrome (ARDS).Importantly, extracorporeal membrane oxygenation (ECMO) is a technology that relies on instrumentation to support the basic needs of the patients, such as severe ARDS patients.However, active hemorrhage has been considered as a contraindication for ECMO treatment in DAH. In recent years, it has been reported that early initiation of ECMO along with a conserved anticoagulation strategy has significant benefits in these patients. Here, we report a successful case of AAVinduced DAH patient who recovered from after venovenous(VV)-ECMO.
CASE
A 14-year-old adolescent with no specif ic family history or past medical history was admitted to the local hospital presenting with cough for 5 d, which progressed to dyspnea and hemoptysis after 3 d. She was then transferred to our department with respiratory distress, continuous hemoptysis,and hematuresis. On arrival, her initial blood pressure was 60/36 mmHg (1 mmHg=0.133 kPa), heart rate (HR) 135 beats/min, respiratory rate (RR) 35 breaths/min, and body temperature 38.1 ℃. High-flow oxygen inhalation was required to maintain oxygen saturation to approximately 80%. Physical examination revealed that chest auscultation was remarkable for rhonchi throughout both lungs and cardiac auscultation was notable for tachycardia with no gallop, rub, or murmurs. The skin was pale and dry, without peripheral edema. The initial arterial blood gas (ABG)revealed respiratory failure and severe metabolic acidosis(pH 7.12, partial pressure of oxygen [PaO] 48 mmHg,partial pressure of carbon dioxide [PaCO] 32.6 mmHg,base excess [BE] –18.5 mmol/L, HCO10.9 mmol/L)and fraction of inspired oxygen (FiO) 100%. Laboratory tests revealed: blood urea nitrogen (BUN) 52.95 mmol/L,serum creatinine (sCr) 1,140 μmol/L, Na130.8 mmol/L,K6.1 mmol/L, white blood cell (WBC) count 23.5×10/L,hemoglobin (Hb) 49 g/L, and platelet count (PLT) 473 ×10/L. A chest computed tomography (CT) scan showed diff use ground-glass opacities suggestive of ARDS, which revealed diffuse pulmonary consolidations suggestive of massive alveolar hemorrhage (Figures 1 A and D). Therefore, the patient was hospitalized to the emergency intensive care unit(EICU) immediately.
While at the EICU, the patient required vasopressor infusion (noradrenaline 0.05 μg/[kg·min]), which was accompanied by worsening hypoxemia. Then, she was intubated and placed on mechanical ventilation. Despite typical ARDS treatment, the patient had progressive hypoxemia with a low PaO/FiO(P/F) ratio of 65, a high plateau pressure of 32 cmHO (1 cmHO=0.098 kPa),minute volumes of approximately 3 L, and poor lung compliance. Therefore, a decision was made to launch VV-ECMO support. An initial sweep gas f low rate of 3.9 L/min with 100% fraction of delivered oxygen improved both oxygenation and ventilatory parameters. ABG after ECMO showed pH 7.45, PaCO32.1 mmHg, and PaO89 mmHg. Due to severe anemia and active pulmonary hemorrhage, 6 units of red blood cells (RBCs) were transfused, and anticoagulation was started for 4 h after cannulation. Heparin was used to maintain the activated partial thromboplastin time (APTT) between 45 s and 60 s, which was less than standard. ECMO allowed for an ultra-protective ventilator strategy involving a tidal volume (TV) of 120 mL (3 mL/kg of ideal body weight),RR of 10 breaths/min, a driving pressure of 10 cmHO,and prone positioning. On the following 5 days, prone positioning was conducted 16 h/day.
To explore the primary cause of the patient, serum ANCA serology showed anti-MPO antibody and perinuclear ANCA (p-ANCA) positive, whereas antiglomerular basement membrane (anti-GBM) and antinuclear antibodies, complement levels, hepatitis,human immunodeficiency virus (HIV) serologies, and blood cultures were all negative. Eventually, AAV was diagnosed on the third day after admission. Therefore,we treated the patient with methylprednisolone pulse therapy (1,000 mg intravenously daily for 3 d) combined with intravenous immunoglobulin (0.4 g/kg per day for 5 d), and continuous hemof iltration was also initiated.
The patient’s situation was improved, which was evidenced by a second chest CT scan (Figures 1 B and E). ECMO was removed after 7-d treatment, and after this, ventilation was also gradually removed. At the time of discharge from the EICU (13day), the chest CT showed a gradual improvement of pulmonary ventilation and reabsorption of the alveolar hemorrhage(Figures 1 C and F). The patient was transferred to the nephrology department and underwent a kidney biopsy,which showed diffuse crescentic glomerulonephritis.The patient was f inally discharged on day 30. At her last outpatient follow-up, she had no respiratory symptoms in room air, but maintained tapering doses of prednisone,and required long-term hemodialysis three times per week.
DISCUSSION
The presentation of DAH is non-specific, ranging from acute respiratory to a more insidious course. Alveolar capillaries rupture into alveoli, which rapidly fill with blood leading to severe ARDS. A retrospective study has been performed, which included 39 patients with immune DAH, and the main cause was AAV (74.3%). Mortality was higher in patients who required dialysis (50.0% vs. 15.4%,=0.045), with oxygen saturation (SaO) 90% at admission(50.0% vs. 5.3%,=0.003) or who required mechanical ventilation (76.9% vs. 6.8%,≤0.001).The above three high-risk factors were all present in our case.
Several previous cases have shown that ECMO is a crucial salvage therapy in patients with DAH.Lung injury may be further exacerbated by spontaneous breathing eff orts and patient-ventilator desynchrony with a consequent increase in transpulmonary pressure in DAH associated with severe and persistent hypoxemia. The lower TV (e.g.,<4 mL/kg) and plateau pressures (e.g., <25 cmHO) were referred to as ultra-lung-protective ventilation in clinical practice. Recently, Rozencwajg et alreported that ECMO allowed ultra-protective ventilation to decrease ventilatorinduced lung injury in severe ARDS. Furthermore,prone position is another important intervention for lung protection, as this positioning could help eliminate lung overdistention by increasing alveolar recruitment, thereby improving oxygenation. Blood drainage is also encouraged by the prone position — the natural drainage position of the superior segment of the lower lobes, which promotes lung recruitment.In the present case, oxygenation improved gradually over f ive continuous days with prone positioning.
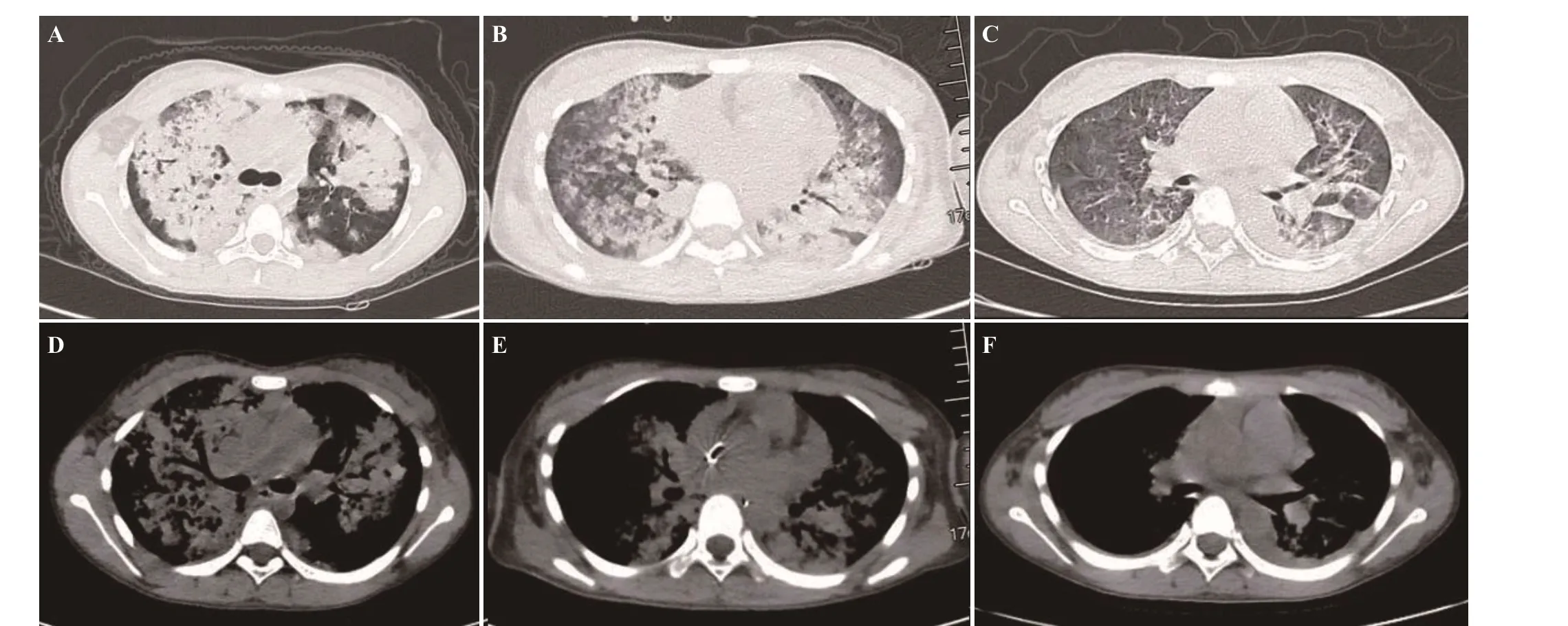
Figure 1. Chest computed tomography images. A and D: two hours before VV-ECMO cannulation, multiple plaque-like high-density shadows were found in both lungs, including ground glass densities, and the margins were unclear; B and E: ECMO combined with prone positioning for f ive days revealed gradual improvement of respiratory function; C and F: at ICU discharge, high-density patches were clearly absorbed. VVECMO: venovenous extracorporeal membrane oxygenation; ICU: intensive care unit.
In patients with DAH requiring ECMO, the anticoagulation therapy is a challenge. Data from the Extracorporeal Life Support Organization (ELSO)document bleeding as a major non-ECMO circuit-related complication. Specif ically, surgical incisions and cannulation sites had the highest bleeding rates with 19.1% and 17.1%,respectively. The systemic anticoagulation is generally considered an essential part of ECMO circuit management,and the potential for serious thromboembolic events is well established.The use of systemic anticoagulation carries significant risks, such as new and increased bleeding.However, ECMO has been used successfully in both pediatric and adult patients with refractory hypoxemia from pulmonary hemorrhage, as evidenced by many studies,which are summarized in the supplementary Table 1. A tenyear retrospective analysis demonstrated that VV-ECMO in refractory respiratory failure due to DAH was feasible.Impressively, Abrams et alreported that the use of ECMO without systemic anticoagulation for 130 d resulted in no catastrophic thrombotic complications. In this regard, the patient did not receive any anticoagulant in the initial 4 h of ECMO. For the subsequent treatment, the anticoagulation target was APTT in 45–60 s. Ultimately, no thrombosis or exacerbation of alveolar hemorrhage occurred, and the active bleeding during ECMO supported the current case.
CONCLUSION
ECMO with anticoagulation strategies and ultra-lungprotective mechanical ventilation may be feasible and effi cient in patients with DAH and ARDS induced by AAV.
The study was supported by Nanjing Medical Science and Technology Development Program (YKK19065; YKK 20075).
Not needed.
The authors have no conf lict of interest.
All authors have substantial contributions to the acquisition, analysis, or interpretation of data for the work; and f inal approval of the version to be published.
All the supplementary files in this paper are available at http://wjem.com.cn.
