Associated risk factors for post-COVID-19 mucormycosis at a tertiary care centre: A cross-sectional study
Praphull Deepankar, Govind Kumar, Jyoti Kr Dinkar, Rishav Mittal
Indira Gandhi Institute of Medical Sciences, Patna, India
ABSTRACT Objective: To explore risk factors of mucormycosis in COVID-19 recovered patients.Methods: A total of 101 patients, who were diagnosed with mucormycosis after recovery from COVID-19 and admitted to the Indira Gandhi Institute of Medical Sciences, Patna, a tertiary care hospital in India, were included in the study. The presenting clinical features and associated risk factors were assessed and analyzed subsequently.Results: Of 101, 68 (67.3%) were males, and 33 (32.7%) were females. A total of 89 (88.1%) patients were between 46 and 65 years old. The most common subtypes were rhino-ocular (61.4%), followed by paranasal sinuses (16.8%), rhino-ocular cerebral (16.8%), ocular (3.0%), and pulmonary (2.0%). Diabetes mellitus was present in 71% of cases of mucormycosis as co-morbidities. A total of 76.2% of patients were given systemic corticosteroids in oral or intravenous form during COVID-19 treatment. Severe COVID-19 was present in 45.5% of patients with mucormycosis, while the moderate infection was present in 35.6% of mucormycosis. Most patients had gap between the onset of mucormycosis and COVID-19 <15 d. Conclusions: A lethal confluence of uncontrolled diabetes mellitus, corticosteroid usage, and COVID-19 could cause a dramatic rise in mucormycosis. So, clinicians must be aware of these risk factors in patients suffering as well as recovering from COVID-19 to prevent mucormycosis.
KEYWORDS: Mucormycosis; COVID-19; Risk factors; Diabetes mellitus; Corticosteroid usage
1. Introduction
Mucormycosis has emerged as a life-threatening complication during the second wave of the pandemic caused by severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) worldwide, especially in India[1]. The prevalence of mucormycosis is low, affecting 0.005 to 1.7 per million populations globally. But in Indian populations, its prevalence is 80 times higher, according to the current data from 2019-2020[2].
Mucormycosis is an angioinvasive disease with a fatal prognosis. It is a fungal disease and its causative fungi belong to the Mucorales order. In this order, Rhizopus, Mucor, and Rhizomucor are important examples. Rhizopus oryzae is a commonly isolated fungus. It is associated with approximately 60% of cases in humans. The mode of transmission in humans is the spread of fungal spores through the respiratory system[3].
Various risk factors are studied for the onset of mucormycosis. These risk factors are diabetes mellitus (DM) with or without its acute complications, use of systemic corticosteroids, underlying malignancies, organ transplantation or other immunosuppressive therapy, acquired immunodeficiency syndrome, morbid obesity, and malnutrition. In COVID-19 patients, immune dysregulation, including cytokine storm, is the primary pathogenesis for secondary infections, including fungus[4].
In COVID-19 recovered patients, associated causative factors for the development of mucormycosis could be DM, obesity, use of corticosteroids, and elevated inflammatory markers. Several studies came out with different hypotheses for the onset of mucormycosis in these patients like high blood sugar (DM, corticosteroid associated, or newly diagnosed DM), presence of environment of low oxygen, metabolic acidosis, and compromised phagocytic functions of leucocytes secondary to suppressed immunity (SARS-CoV-2 virusmediated, or due to delayed recovery[5]. Several assumptions also surfaced during the mucormycosis pandemic, like poor quality of oxygen piping and transport system, poor maintenance of water in oxygen flowmeter, and use of industrial oxygen[6]. Nasal and oral mucosal injury is expected due to repeated use of steam inhalation or high flow oxygen. This mucosal injury is helpful for fungus colonization[7].
This is among the few studies from India which discusses the important risk factors for the onset of mucormycosis in COVID-19 recovered patients and its clinical profile.
2. Patients and methods
2.1. Study setting
In this observational study, we evaluated the patients from the Inpatient Department of Indira Gandhi Institute of Medical Sciences, Patna, India, with the diagnosis of mucormycosis between 15 May 2021 and 30 July 2021.
2.2. Ethical statement
Ethical committee approval was taken for this study (No. 290/IEC/IGIMS/2021.).
2.3. Inclusion and exclusion criteria
All cases of mucormycosis were diagnosed histopathologically with COVID-19 in the recent past. And patients having negative or unknown RT-PCR/rapid antigen tests for SARS-CoV-2 were excluded from the study.
2.4. Measurements
After enrollment, defined clinical data of participants, including sex, age, coexisting disease, clinical symptoms, the time between COVID-19 & onset of mucormycosis, and severity of COVID-19 were recorded and analyzed.
2.5. Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences program (SPSS v25) for Windows. For statistical analysis, we used frequencies and percentages to describe categorical variables. The data presentation was done as number (%). The inter-group statistical comparison of the distribution of categorical variables was tested using the Chi-square test. The significant level of this study was set at α=0.05. P-value equal to or less than 0.05 was considered statistically significant.
3. Results
One hundred one patients with mucormycosis were included from In-patient Department of the Indira Gandhi Institute of Medical Sciences, Patna (Bihar), India (Figure 1).
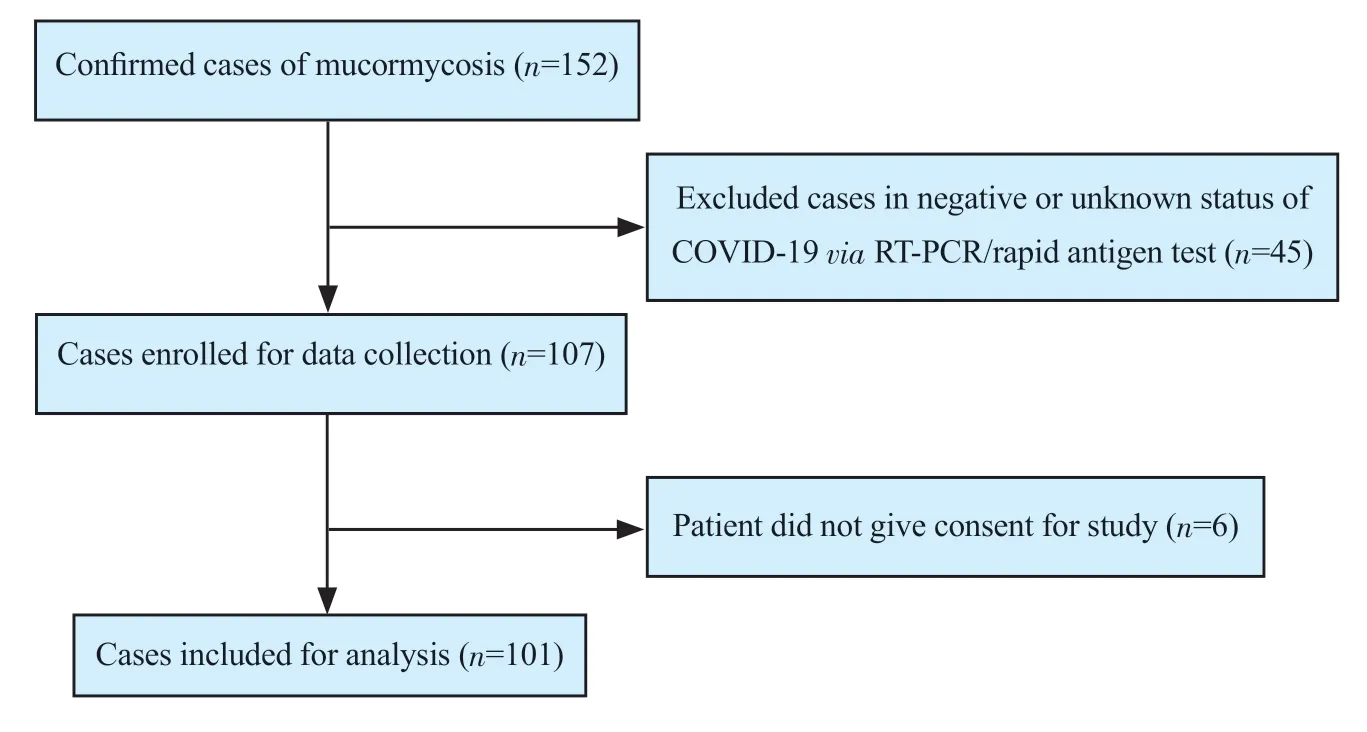
Figure 1. The study flowchart.
Out of 101 patients, 67.3% (n=68) were male and 32.7% (n=33) were female. The majority of patients (n=89, 88.1%) were between 46 to 65 years of age (Table 1).
Most patients presented with rhino-ocular involvement (61.4%), followed by paranasal sinus (16.8%) and others (Table 1). The major comorbidities were DM alone or with its complications (69.3%) followed by hypertension (21.8%) (Table 1). Among other risk factors, the use of systemic steroids (oral or intravenous) was noticed in 76.2% (n=77) of mucormycosis patients. In these patients, 44.6% (n=45) were given steroids more than 14 d, while 24.8% (n=25) were given for for 7-14 d (Table 2).
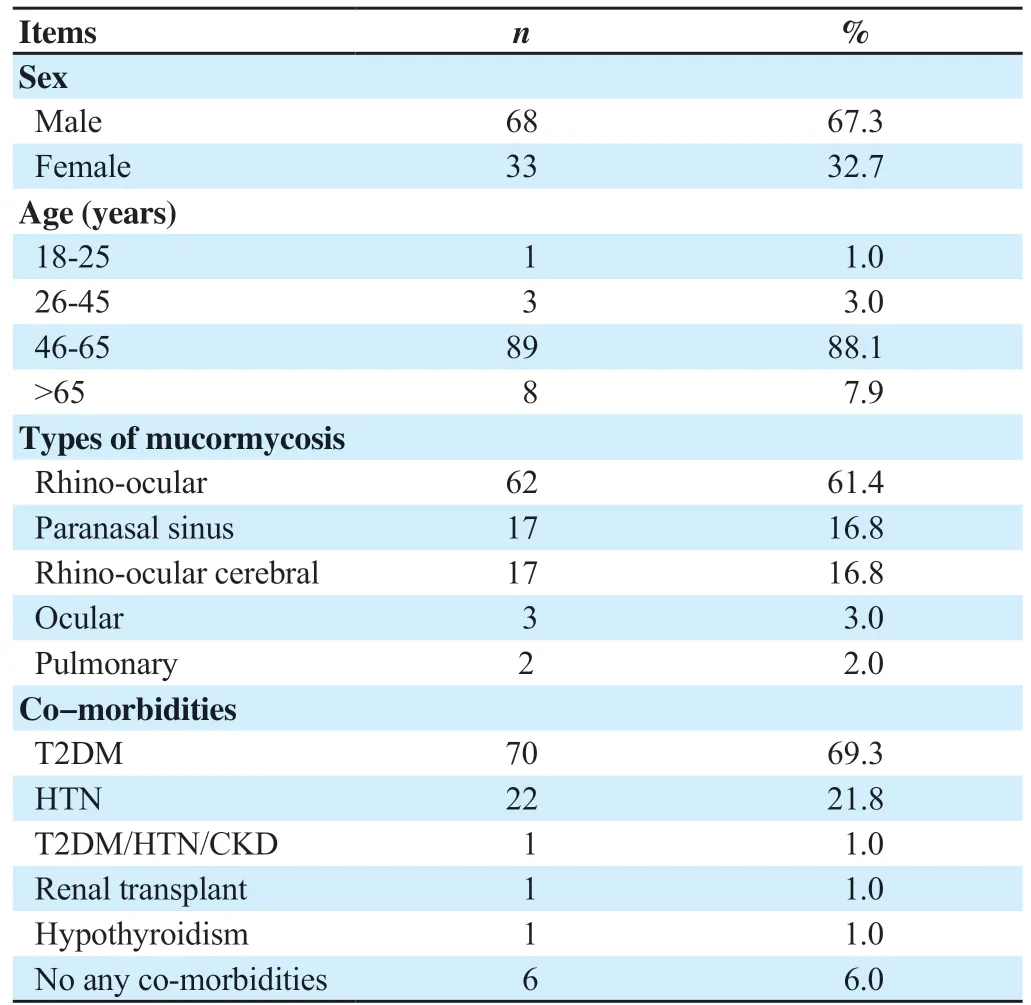
Table 1. Demographic and baseline characteristics of the study patients (n=101).

Table 2. Systemic steroid use, oxygen requirement during COVID-19, and time between mucormycosis and COVID-19 (n=101).
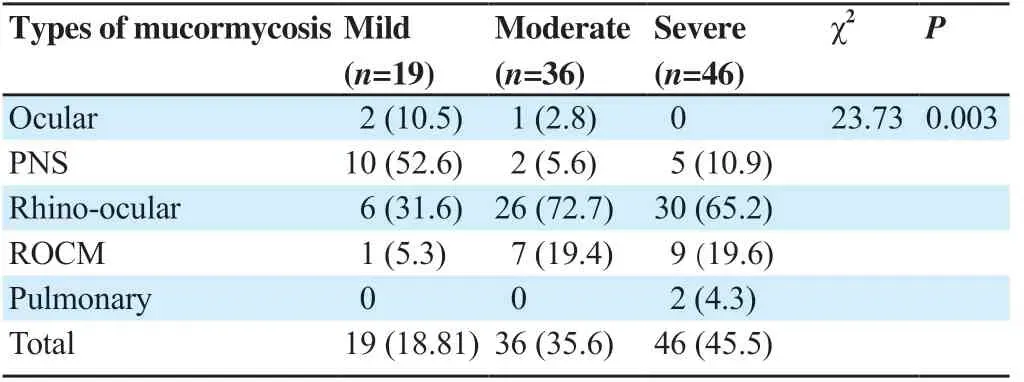
Table 3. Types of mucormycosis with severity of COVID-19 infection (n=101, n, %).
Oxygen therapy was given to 73 patients with mucormycosis for the treatment of COVID-19 pneumonitis (Table 2). In 53.5% of patients, the gap between the onset of mucormycosis and COVID-19 was less than 15 d, followed by 15 to 30 d in 33 individuals (32.7%) (Table 2). Severe COVID-19 infection was found in 45.6% of cases, while mild COVID-19 was found in 18.8% of patients (P<0.05)(Table 3).
4. Discussion
Mucormycosis is not a new disease. It mainly occurs in patients with impaired immune systems like DM. It has become a fatal complication of COVID-19 in the second wave of the pandemic. Mucormycosis was declared a notifiable disease in India during this period[8,9].
Mucormycosis may present as different clinical subtypes based on site of involvement like ocular, paranasal sinuses, rhino-ocular, rhino-ocular cerebral, pulmonary, jaw bone, and others. Rhino-ocular mucormycosis is the common type reported in clinical practice worldwide[4]. In a meta-analysis, Patel et al. also described rhinoocular mucormycosis as a major type (67.7%) of mucormycosis[10]. Our study also finds similar results. In another study by Chakrabarti et al., the most common subtype was rhino-orbital-cerebral mucormycosis, and pulmonary was the second most common form during the second wave[11]. But we found rhino-orbital-cerebral mucormycosis as the second most common type of mucormycosis after rhino-ocular.
Among all the risk factors studied, DM is described as a major comorbidity in various literature like ours. Patel et al. reported DM as a co-morbidity in 70% of patients[10]. In our study, DM is present in 71% of cases.
Importantly, the COSMIC, a multicentric epidemiological study, showed over 65% of post-COVID-19 mucormycosis had uncontrolled diabetes. And they described diabetes mellitus as the most significant risk factor[12]. Decreased immunities as a result of diabetes and COVID-19 make the patients susceptible to secondary infections. In a systemic review of 15 studies, DM is found as an important risk factor for post-COVID-19 mucormycosis. They briefly discussed the role of hyperglycemia control in the management of both COVID-19 and mucormycosis[13]. In a recent systematic review, John et al. observed that diabetes was in 93% of cases of post-COVID-19 mucormycosis[14].
Another important risk factor studied in different works of literature is the use of corticosteroids in COVID-19 treatment. Systemic corticosteroids were used inappropriately in dose and duration. In our study, systemic steroids were used either in the oral or parental form in 76.2% of patients. A study from western India reported a total of 3.36% (32/953) patients from COVID care center developed mucormycosis, and 93% of them had been given corticosteroids during treatment of COVID-19[15]. Patel et al. found that 71.4% of patients with mucormycosis had exposure to systemic corticosteroids in a systemic review[12]. John et al. have observed that diabetes mellitus was there in 93% patients of mucormycosis, and systemic corticosteroids were given to 88% of patients during COVID-19 treatment in a recent systematic review[14].
In our study, more patients used oxygen less than 7 days. Singh did not find any association between the duration of oxygen use and the development of mucormycosis either[1]. We noticed the cases of mucormycosis were higher in patients with severe COVID-19 than in mild and moderate ones. This is similar to the study of Patel et al[12].
In a study by Bhogireddy et al., tocilizumab, an IL-6 antagonist used in patients with COVID-19 for managing cytokine storm, is described as a risk factor for mucormycosis[16]. Although we didn’t find any case of mucormycosis where tocilizumab was used in the past.
Most of the studies found that the duration between the onset of mucormycosis and SARS-CoV-2 infection was 10-15 d[11]. This mean duration was (15.6±9.6) d in a study by Sen et al[17]. In our study, most patients had gap between the onset of mucormycosis and COVID-19 <15 d.
DM and corticosteroids are two risk factors consistently associated with mucormycosis development after SARS-CoV-2 infections. However, we need comparative observations for the development of mucormycosis in non-diabetic and diabetic COVID-19 patients with or without the use of corticosteroids in further study. More research is required to understand how COVID-19 contributes to the emergence of mucormycosis.
Mucormycosis has been identified as fatal sequelae of COVID-19. The Mucorales order is the cause of this uncommon fungal infection. It may have been classified based on sites like ocular, paranasal sinus, rhino-ocular, rhino-ocular cerebral, pulmonary, and others. Rhino-ocular is the most common type in our study. The important risk factors studied are DM, the severity of COVID-19, and corticosteroid use. The most prevalent co-morbidity among mucormycosis patients is DM. It is advised to regulate uncontrolled blood glucose strictly to minimize complications of COVID-19, and only judicious use of corticosteroids should be advised to prevent mucormycosis.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Authors’ contributions
D.P. participated in study design, analysis of data, and drafting of the manuscript. K.G. supervised study design, and analysis of data and performed critical revision and decision on the final manuscript. M.R. collected the data and participated in drafting the manuscript. D.J.K. contributed to the literature search, data collection and analysis. All authors reviewed the results and approved the final version of the manuscript.
 Journal of Acute Disease2022年4期
Journal of Acute Disease2022年4期
- Journal of Acute Disease的其它文章
- Challenges of COVID-19 prevention and control: A narrative review
- Delayed post-hypoxic leukoencephalopathy following barbiturate overdose: A case report
- Severe progression of autoimmune hepatitis in a young COVID-19 adult patient: A case report
- Hematological indices as predictors of mortality in dengue shock syndrome: A retrospective study
- Different routine laboratory tests in assessment of COVID-19: A casecontrol study
- Effect of oral premedication of midazolam, ketamine, and dexmedetomidine on pediatric sedation and ease of parental separation in anesthesia induction for elective surgery: A randomized clinical trial
