Evaluation of the intervention of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease
Ye Zhng, N-Ping Xu, Bei-Rong Mo, Xin-Ling Liu, Y-Chng Lin
aUnion Medical College, Huazhong University of Science and Technology, Shenzhen, Guangdong 518000, China
bShenzhen University, Shenzhen, Guangdong 518000, China
Abstract: Objective: Chronic obstructive pulmonary disease (COPD) can be prevented and treated, although presenting with persistent airflow restriction; the airflow restriction caused by COPD is mostly progressive. In recent years, more attention has been paid to the homebased pulmonary rehabilitation (PR) and its influence on COPD. Exercise training is the basic constituent of PR. However, it is not clear which exercise trainings are the ideal ways to deliver home-based PR.
Keywords: chronic obstructive pulmonary disease ? exercise training ? home-based pulmonary rehabilitation
1. Introduction
According to the study published by the World Health Organization, chronic obstructive pulmonary disease(COPD) is expected to account for the fifth place in the world’s economic burden by 2020.1–3COPD is a common disease with persistent airflow restriction that can be prevented and treated, and its airflow restriction is mostly progressive.4The main symptoms of COPD are dyspnea, fatigue and reduced physical activity,progressive aggravation, and spiral of symptoms,which seriously affect the patient’s labor and quality of life.5,6Therefore, pulmonary rehabilitation (PR) has become an important part of the treatment of patients with COPD.6,7
PR has become the most effective nondrug intervention in improving kinetics and the state of health in patients with COPD, even in the presence of very severe disease condition.8An increasing number of reports show that supervised and trained PR programs improve endurance of muscle exercise, quality of life, activity of daily life, respiratory symptoms,and dyspnea. However, regular visits to hospitals or clinics may result in a patient’s inability to comply with or reduce compliance, which is often a primary obstacle to the success of these programs. Another approach, therefore, is to consider a home-based rehabilitation program, which may be an effective way of delivery.
Recently, some systematic reviews of the research focus on the effectiveness and safety of home-based PR inpatients with COPD.9,10The results of some reviews show that home-based PR program can be an effectual, easy, cheap, and effective program to reduce fatigue and improve abilities of daily living (ADL) and quality of life (QOL) in COPD patients. Movement training is the basis of PR and is the effective method to improve the muscle function and chronic respiratory symptoms in patients with COPD.11,12However, those reviews did not focus on interventions of home-based exercise training.What kind of PR exercise intervention can not only achieve certain rehabilitation effect but also be better accepted by patients, to improve exercise compliance? Through the analysis of 21 selected articles,we classified these PR interventions and studied the rehabilitation effects of different intervention methods on patients. Therefore, the innovation of this study is to: (i) discuss the current family movement training for patients with COPD from the aspects of intervention type, content, method, and results; and (ii) provide the basis for the direction of the future family rehabilitation research.
2. Methods
2.1. Search and select procedures
Search for literature on home-based PR. The keywords used are “COPD,” “COAD,” or “chronic obstructive pulmonary disease” and “home-based pulmonary rehabilitation.” It includes four relevant databases (PubMed,Web of Science, Medline, and China National Knowledge Infrastructure) established from January 2008 to January 2018. According to the predetermined selection and exclusion criteria, the qualification and selection of the article are evaluated by screening and obtaining the complete text. The selection procedures of studies are presented in a PRISMA flowchart (Figure 1).
2.2. Inclusion and exclusion criteria
The research included in this review must meet the following criteria: articles published in English or Chinese(the language used by the author) were searched in four databases from June 2008 to June 2018. The study focused on home-based lung-rehabilitation interventions and measured results in patients with COPD. Reviews,editorial, literary reviews, and conference papers are not included in this review.
The criteria for inclusion in this review were:
Focuses: (1) patients with COPD, (2) home-based PR, and (3) articles published from 2008 to 2018.
Type of studies: RCT
The criteria for exclusion were (1) editorial, (2) literature review, (3) PR not at home but in community or hospital, (4) focus on self-management, and (5) patients without COPD.
The selection procedures of studies are presented in a PRISMA flowchart (Figure 1).
2.3. Appraisal of the quality of the included studies
The “bias risk” of Cochrane collaboration was used to appraise the quality and bias risk of each article included in RCT. The tool assessed seven specific domains: generation of the random sequence, assignment of concealment,blindness for the subject and the intervention provider,blind method of the results assessment, incomplete data,and selectivity of the result report, which can be assessed as “l(fā)ow-bias risk,” “high-bias risk,” or “not clear bias risk.
According to the judgment standard criteria (Cochrane Handbook for Systematic Reviews of Intervention. Part 2:8.5), in the case of a systematic review of the intervention, if there is no data in the test, further information can be collected by contacting the original author.
2.4. Statistical analysis
The meta-analysis was performed using ReviewManager5.3 software provided by the Cochrane Collaboration. If data cannot be converted or merged, a descriptive analysis is used.
2.5. Data extraction and quality evaluation
In the initial extensive search, the two reviewers separately evaluated the titles and abstracts of all potentially germane articles by strictly complying with the inclusion/exclusion criteria and the differences in research options.The two researchers independently extracted the following data from all included studies: health-related quality of life (HRQOL) score, dyspnea, exercise ability, exercise tolerance, pulmonary function, anxiety and depression, adverse events, etc. They resolved the differences through discussions until a consensus was reached.
3. Results
3.1. Characteristics of the interventions
All 21 studies focused on home-based PR interventions in 14 countries and regions, namely, the USA(n= 3, 14.3%), China (n= 2, 9.5%), Taiwan (n= 2, 9.5%),Spain (n= 2, 9.5%), Brazil (n= 2, 9.5%), The Netherlands(n= 2, 9.6%), Australia (n= 1, 4.8%), Germany (n= 1,4.8%), Iran (n= 1, 4.8%), Italy (n= 1, 4.8%), France(n=1, 4.8%), UK (n= 1, 4.8%), Britain (n= 1, 4.8%), and Japan (n= 1, 4.8%). The 21 studies were randomized controlled trials (Table 1).
3.2. Target population
In these studies, the size of the sample ranged from 20 to 287 patients, with a total of 1694 patients. The wear rate is 0–49.5%, with an average of 23.6%(400/1694). The reasons why patients refuse to participate in or withdraw from home-based PR are (1)the causes of illness, such as acute exacerbation of COPD or deterioration or complications, or suffering from another illness or death, which affects PR training,13–27(2) loss of visit,15,18,21–23,28and (3) lack of cooperation.15–17,21,22,24,27,28There are also other factors,such as time conflict,14difficulty in operating instruments,13and entering into another maintenance procedure.17There are also traffic problems in central PR.13Some articles only mention the number of dropouts without explaining the reasons for dropping out.29–32One article mentions that one dropout is due to death,whereas others do not explain the reasons for drop out.27Another article33does not explain dropouts. Most of the home-based PR patients in these intervention studies were middle-aged and elderly, ranging in age from 40 to 80 years. Two other articles dealt with young and middle-aged people whose age requirements were >18 years (Table 1).
3.3. Theoretical framework of the interventions
Most of these theoretical frameworks focused on the comparison of two PRs, including the home-based pulmonary and the central-based PR,15,16,21,22,28and the home-based PR13,14,17–20,23–27,29–33Moreover, there is an article that compares home-based PR with centralbased PR and family routine rehabilitation.32In these articles, the control group’s family routine rehabilitation usually refers to conventional treatment care with or without respiratory training. Routine treatment care refers to drug therapy and health education. Drug therapy refers to the use of bronchodilators, anticholinergic drugs, cough relieving expectorant drugs, and so on.Health education refers to COPD’s disease knowledge,smoking ban, diet, medication, prevention and treatment of acute attack, rest, and so on. Breathing training usually refers to lip breathing and abdominal breathing.The control group family/central PR involved in these articles refers to the addition of some rehabilitation exercises on the basis of conventional rehabilitation, such as aerobic exercise, endurance training, upper limb exercise (ULE), lower limb exercise (LLE), and relaxation training (Table 1).
3.4. Intervention approaches and focuses
The mode of intervention can be divided into two major categories, namely regulatory15,18–22,24–33and unsupervised,13,14,16,17,23with supervision including: telephone supervision—checking and urging patients’ to exercise through regular telephone conversations; follow up regularly—physical therapists visit home regularly to check the condition of patients’ exercise and give further guidance to them.19,26,27,29,31Time supervision meeting—patients do diary records at home, and regularly return to the center to meet with physiotherapists.18,20Unsupervised—usually refers to the unified guidance to the patient before the intervention and giving out the pamphlets; the patient exercises according to these instructions at home, during the no-appointment period. What form of supervision is followed?The means of interventions are divided into instrumental13–15,17,18,26–28,30and noninstrumental.16,19–25,29,31–33Instrumental assistance generally includes the following elements: walking with endurance to the music on a cell phone or other instruments for maximum endurance walking13,14; walking through a pedometer which17,26provides guidance, this instrument is also used to detect heart rate28; combining with home ventilator to carry out PR18,27; inhalation and atomization inhalation30; and lending portable ergo cycles that could adjust the resistance manually.15No instrumental assistance usually refers to PR exercises without any instrumental assistance (Table 1).
3.5. Dosage of interventions and follow-up time frame
In some articles, the duration of intervention is about 28.6 min (ranges from 15 to 70 min) with an average frequency of 4.7/week (range 2/week 7)14–19,21–25,27,32,33; some articles determine the duration of each exercise based on the intensity of the set of exercise targets;13,26,28,31and in some articles, the intervention changes and adjusts according to the tolerability of subjects.20,29,30
Different follow-up period also showed in the Table 1: 12 months (n= 5, 23.8%), 6 months (n= 4,19%), 4 months (n= 1, 4.8%), 3 months (n= 5, 23.8%),2 months (n= 3, 14.3%), 10 weeks (n= 1, 4.8%), and 7 weeks (n= 2, 9.5%).
3.6. Delivery of interventions
The intervention in these articles with or without supervision is trained by a physiotherapist or professional medical staff, and all these studies have formulated and followed a special intervention program and included regular checks in the entire intervention program to maintain the standard of treatment.
The intervention of the nearly 1/3rd of the articles was delivered to the combination of the intervener and the patient’s face-to-face and telephone conversation,and nearly 1/5 (n= 4, 19%) was delivered with a combination of face-to-face and diary contacts between the intervener and the patient; and the intervention of the nearly 1/5thof the articles was delivered to the intervention group with three groups of face-to-face, telephone, and diary contacts with the patient. Combined to deliver (n= 4, 19%), there are other interventions that are delivered by the intervener to the patient’s face-to-face (n= 3, 14.3%) and the diary to contact(n= 2, 9.5%), respectively; in addition, the intervention of an article26is delivered to the log of the pedometer(n= 1, 4.5%) (Table 1).
3.7. Outcomes of the intervention
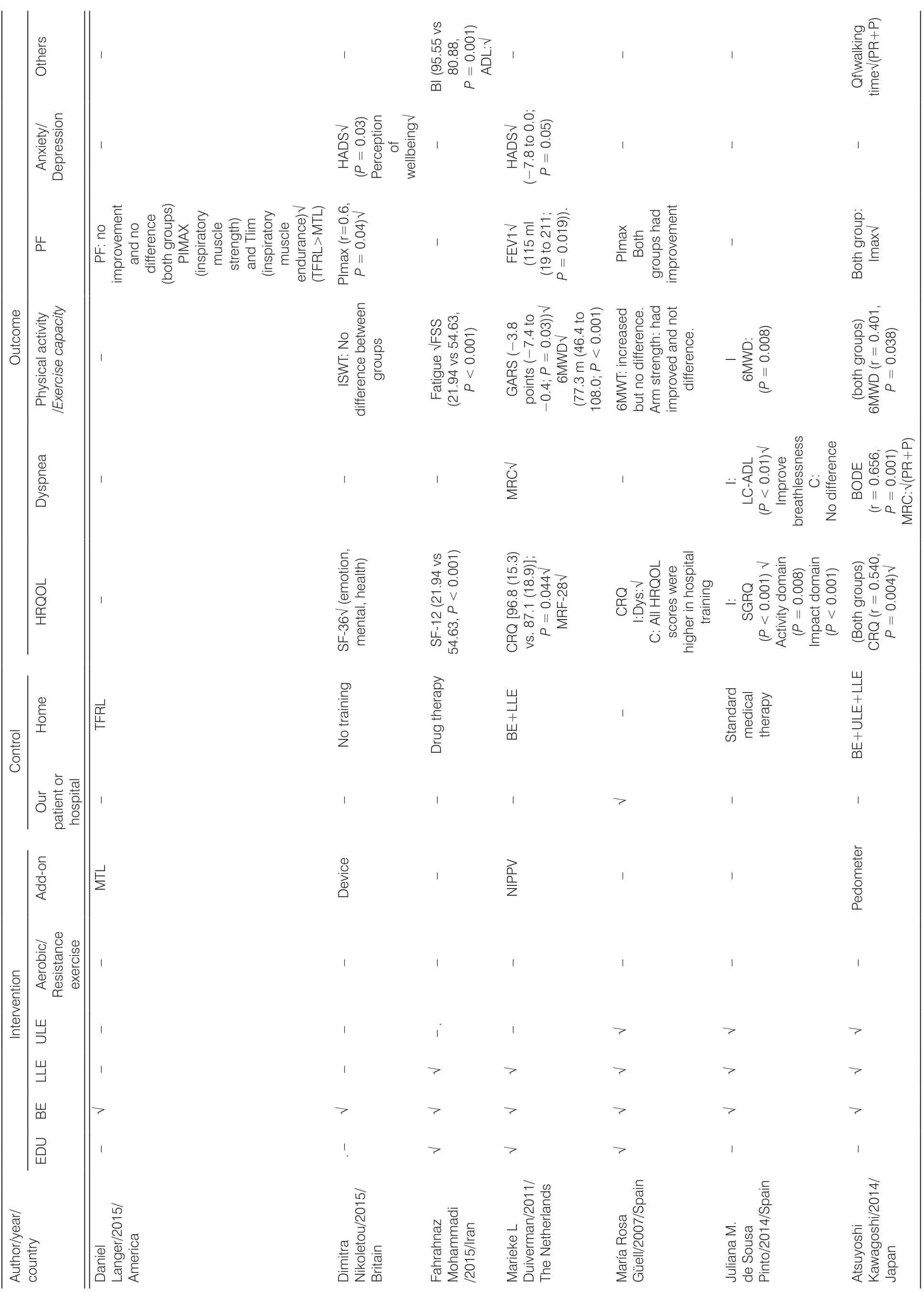
3.7.1. Inspiratory muscle training program
Two of the RCTs report means of intervention of inspiratory muscle training (IMT) program. One of the trials showed that multiple tests have evaluated the change in muscle function after IMT, with greater cohesiveness.31
The other trial was to compare the effects of traditional IMT or TFRL regimens on the function of the inspiratory muscle in patients with COPD. The result showed that the short-term and home-based IMT scheme can effectively improve the function of inspiratory muscle in both groups. Compared with MTL group, the subjects of the TFRL group were subject to higher training load, and the function of the inspiratory muscle was significantly improved.20All of the trials reported significant improvement on inspiratory muscle function through the IMT intervention (Table 2).
3.7.2. Lower limb exercise program
There are 6 RCTs that use LLE training alone in family lung-rehabilitation such as walking training.There were two studies that assessed daily endurance walking by following the rhythm of music with an 80% oxygen uptake (VO2) from a program installed on a mobile phone. The results showed that the Incremental Shuttle Walking Test (ISWT) distance and endurance walking time in the intervention group were significantly improved. ISWT distance, inspiratory ability, and quality of life continued until the end of the study, whereas acute aggravation period and hospital stay decreased.13,14Four of the trials compared home-based intervention with the usual care,and the results indicated that home-based LLE with or without add-on intervention was more effective (measured by CRQ, SGRQ, ISWT, etc.) than the usual care.13,14,17,27Compared with center-based interventions, two trials showed that standardized family rehabilitation programs were comparable and not inferior to supervised central rehabilitation programs.22,23One trial showed that noninvasive intermittent positive pressure ventilation (NIPPV) in patients with COPD was significantly improved compared with routine treatment27(Table 2).
3.7.3. Breathing exercise and lower limb exercise programs
Two of the RCTs reported the intervention of breathing exercise (BE) and LLE at home.18,33One of the trials found that the average scores of tiredness were evidently lower in the test group (P< 0.001) after home-based PR in the test group, while the average scores of ADL (P< 0.001) and QOL (P< 0.001) were significantly improved after home-based nursing PR in the test group. Home-based PR can be an effective,cheap, and available regimen to decrease tiredness and improve ADL and QOL in COPD patients.33In addition to BEs and LLE, one of the trials reported that adding NIPPV to PR for two years in COPD patients with chronic hypercapnia could improve HRQOL, difficult breathing, hypofunction of lung, mood, and exercise tolerance. As time goes on, the gain is further increased18(Table 2).
3.7.4. Lower limb exercise and upper limb exercise programs
Three of the RCTs reported using upper limb movements and lower limb movements as means of lung-rehabilitation. One of the trials indicated that home-based PR program provided incremental effect by 65 m in the 6MWT (P< 0.05) and 316.6 ± 81.8 m in the endurance test (P< 0.05) and was reduced by>4 units in all SGRQ domains.25Two of the trials indicated that home-based and self-monitoring PR group is as effective as outpatient PR, and it is an effective choice for the treatment of patients with COPD21,28(Table 2).
(continued)
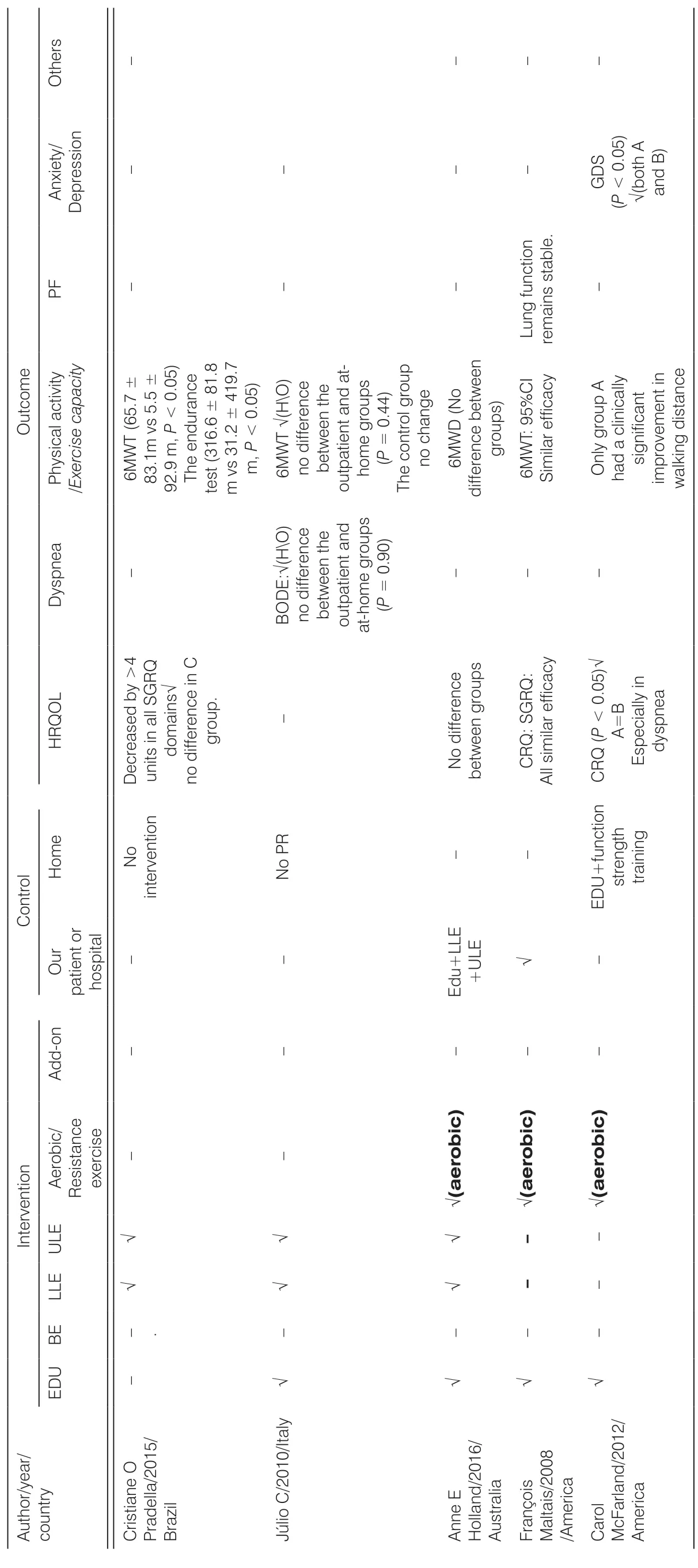
Table 2. Outcomes of home-based intervention of included studies.
3.7.5. Breathing exercise, lower limb exercise, and upper limb exercise programs
Six of the RCTs reported outcome of BE, LLE, and ULE as home-based PR.16,19,24,26,30,32Comparing with hospital training, one trial showed that the standardized home-based program provides benefits in dyspnea.22Five of the trials reported that this intervention provides evidence that home-based PR improves the quality of life, breathing difficulties in daily life, and exercise ability in patients with severe and very serious COPD. It is important to note that patients who are far away from the hospital can be treated using home-based PR as part of the treatment.19,24,26,30,32Among those using BE, LLE,and ULE as home-based PR, one trial reported that the low-intensity HBPR that is fed back with the pedometer is an effective method to improve the PA, where the improvement of the physiological factors is related to the increased walking time of the COPD patient. At the same time, another trial reported that in subjects with severe COPD, a home-based NMES as an addition to PR does not lead to further improvement and may cause a burden to some patients (Table 2).
3.7.6. Aerobic exercise program
Three of RCTs reports the outcomes of aerobic exercise. One pilot study suggested that aerobic exercise and functional intensity training in home PR can improve the quality of life of patients with COPD to some extent.29Two of studies suggested that as a means of home-based PR, the short-term clinical outcome produced by the aerobic exercise with minimal resources can be equivalent to the outcome of the central PR15,21(Table 2).
4. Discussions
Home-based PR is to point to the place that executes PR as a family, because helping a patient to reduce economic costs and save time makes it more feasible.This systematic review of 21 studies is the first to investigate the effect of different home-based exercise trainings on COPD. Some articles show that home-based PR can improve HRQOL, exercise endurance of COPD patients, alleviate breathing difficulties in patients needing PR and bronchodilation, and attenuate the severity of their pulmonary condition. Fatigue and emotional states can also have advantage from home-based pulmonary rehabilitation when patients are unable to receive hospital PR.13,14,24,26,30,32
In this review, we found that daily, simple, structured,self-monitoring, family-based exercise training was an effective, low-cost intervention for the home-based PR program. This is also consistent with some research findings. Previous studies and guidelines have shown that PR is useful to patients with COPD because it can improve motor ability, muscle strength, symptoms, and HRQOL.34Home-based PR is also increasingly being recognized. This review further confirmed the effectiveness of home-based PR in HRQOL, PA, dyspnea, AF,etc. and further studied the effects of all kinds of homebased PR.
The present study has shown the effectiveness of simple, low-cost, low-intensity, home-based PR program that is suitable for causing the actual conditions capable of leading to an improvement in exercise capacity, relief for breathlessness, activities of daily living, and quality of life in patients with COPD. The use of minimal resources in the home-based PR program might result in a clinical outcome equivalent to a center-based PR. Home-based low-intensity aerobic training may sometimes be no less than outpatient or central intervention to improve dyspnea, health, and exercise tolerance. This is consistent with some previous studies.35Although high-intensity training in COPD patients has greater biological benefits than low-intensity training, studies have also shown that low-intensity training can also produce clinical benefits.
LLE training may be the best method of home-based exercise rehabilitation. Whether the primary method of home-based PR is simply LLE or LLE combined breathing training or LLE combined ULE, it can be confidently asserted that LLE training is the most appropriate method of delivering PR. This is consistent with the view in the guidelines for PR, it is stated that LLE training is a key core of PR.34At the same time, it is pointed out in the guide that the recommended evidence for lower limb training is Level A. This shows the importance of LLE training; in addition, LLE training can improve the patient’s exercise endurance and is more convenient to carry out at home. Most of the sports indicated that training for home-based PR mainly consists of lower limb training, such as street walking daily, going up and down stairs, riding a bicycle, etc. and these also achieved better results.14,17,22,23Combined exercise training may be better than single exercise training. This indicates that the combined training program is superior to the LLE training alone.16,24,30Compared with single exercise training, many evidences show that the home-based PR of combined LLE training with breathing training and ULE shows great improvement in HRQOL, dyspnea,physical activity, and lung function.
Adverse events during home-based PR exercise were no more frequent than those in hospital or central nursing, which may be related to better supervision, effective control of exercise intensity, and remote help and follow-up. It is suggested that more objective scientific indicators should be used to control the intensity, frequency, and duration of exercise training to ensure the safety of patients and achieve corresponding results. Under the right conditions, the use of additional measures may have better effects or better compliance,such as music, pedometer, and the use of NIPPV for severe patients.13,14,18This additional factor needs careful study and consideration. Otherwise, it may also be a burden for some patients.32
However, further studies are required. In this review,the sample size of some RCT articles is insufficient. At the same time, the intervention time of home-based PR is a major variable, and it has an important influence on the results of the study. Due to the difference in the intervention time, some indicators cannot be combined,but the improvement will be more pronounced as the intervention continues.
5. Conclusions
The results from the analysis may imply that simple, lowcost, low-intensity home-based PR program is suitable for the actual conditions that might lead to improvement in exercise capacity, relief for breathlessness, activities of daily living, and quality of life in patients with COPD.In particular, LLE training in home-based PR is more significant. At the same time, the combination of LLE training with breathing training and ULE training is more obvious than the simple LLE training. In addition, homebased low-intensity aerobic training may sometimes not be inferior to the outpatient or center intervention to improve dyspnea, health status, and exercise tolerance.
In conclusion, the simple and easy home-based PR exercise program is effective. Long-term home-based PR may require better maintenance strategies, which can benefit patients in the long run.
Ethical approval
Ethical issues are not involved in this paper.
Conflicts of interest
All contributing authors declare that no conflicts of interest exist.
- Frontiers of Nursing的其它文章
- Frontiers of Nursing Call for Papers
- A conceptual analysis of the meaning of comfort at the end-of-life using the Walker and Avant (2014) Framework
- Research on teaching reform of rehabilitation nursing major based on modern apprenticeship system?
- Association between calcium supplementation and bone mineral density in children: a systematic review and meta-analysis
- Evaluation of undergraduate students’ nursing assessment and communication skills through an objective structured clinical examination within a high-fidelity simulation using a student-simulated patient?
- The effectiveness of dalethyne dressings for reducing bacteria in diabetic foot ulcers