Serum non-high-density lipoprotein cholesterol level is increased in Chinese patients with nonalcoholic fatty liver disease
Si-Yu Sho , Yi-Ln Wng , Li-Min Feng , Ying Zho ,*
a School of Laboratory Medicine and Life Science, Wenzhou Medical University, Wenzhou 325035, China
b Department of Clinical Laboratory, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
c Key Laboratory of Clinical In Vitro Diagnostic Techniques of Zhejiang Province, Hangzhou 310 0 03, China
TotheEditor:
Nonalcoholic fatty liver disease (NAFLD) is a growing public health problem globally. Although the primary liver pathology in NAFLD patients is associated with an increased risk of overall mortality, the majority of deaths in NAFLD patients are due to the cardiovascular disease (CVD) [1] . With the change of lifestyle, the prevalence of NAFLD in China is increasing and patients tend to be younger [2] . A relevant epidemiological survey has shown that the prevalence of NAFLD in adults is estimated to be 12%-24%in Asia [3] . Non-high-density lipoprotein cholesterol (non-HDL-C)refers to the sum of all cholesterol subtracts high-density lipoprotein cholesterol (HDL-C), which can more comprehensively reflect the comprehensive metabolic changes of lipoproteins including low-density lipoprotein cholesterol (LDL-C), intermediate-density lipoprotein cholesterol (IDL-C), and very-low-density lipoprotein cholesterol (VLDL-C) [4] . Recently, NAFLD that often coexists with dyslipidemia has been identified as a major modifiable risk factor of CVD, and non-HDL-C has become a new biomarker for assessing and predicting the risk of CVD [4] . Therefore, we used the data from health checkup and examined the relationship between the serum non-HDL-C level and NAFLD.
Our study included 398 NAFLD participants (306 males and 92 females) and 101 non-NAFLD participants (77 males and 24 females) who had a medical health checkup at the First Affiliated Hospital of Zhejiang University School of Medicine between April 2017 and October 2017. NAFLD was diagnosed according to the Chinese NAFLD guideline issued by the Chinese National Consensus Workshop [5] . The patients with alcohol consumption, autoimmune hepatitis, viral hepatitis, and hepatotoxic medications were excluded. Serum biochemical markers were determined using a Hitachi DDP autoanalyzer (Hitachi Corp, Ibaragi, Japan). The differences of baseline and laboratory variables between NAFLD group and non NAFLD group were analyzed using a Kruskal-WallsHanalysis. The correlation between non-HDL-C and other variables was analyzed using the Pearson correlation analysis. The multivariate logistic regression was used to examine the association between the non-HDL-C and the prevalence of NAFLD.
The clinical and laboratorial characteristics were summarized in Table 1 . Significant differences were detected between the NAFLD and non-NAFLD groups with respect to systolic blood pressure(SBP), diastolic blood pressure (DBP), body mass index (BMI),alanine aminotransferase (ALT), aspartate aminotransferase (AST),gamma-glutamyltransferase (GGT), uric acid (UA), glucose (Glu),triglyceride (TG), total cholesterol (TC), creatinine (Cr), HDL-C and LDL-C levels. Compared with the non-NAFLD group, the non-HDLC level was significantly elevated in the NAFLD group (3.87 vs.2.96 mmol/L,P<0.001]. We found that in NAFLD patients non-HDL-C level correlated positively with age, SBP, DBP, BMI, ALT, AST,GGT, UA, Glu, and TG (P<0.05) ( Table 2). Following adjustment for SBP, DBP, BMI, ALT, AST, GGT, UA, Glu and Cr, the multivariate logistic regression analysis showed that serum non-HDL-C level was an independent risk factor for NAFLD (OR = 2.527, 95% CI: 1.345-4.747,P= 0.004).
The non-HDL-C level reflects the damage extent of the coronary arteries and is a more specific marker than a single type of lipoprotein cholesterol to reflect atherosclerosis [ 4 , 6 ]. Some studies showed that non-HDL-C was superior to LDL-C in predicting CVD [ 6 , 7 ]. Patients with NAFLD may present with abnormal lipid metabolism, resulting in increased serum non-HDL-C level and concurrent CVD. NAFLD is related to CVD and cancer [ 1 , 8 ]. Zelber-Sagi et al. [9] revealed that the increased non-HDL-C levels precede the onset of NAFLD, indicating that the impairment of cholesterol regulation may have a causal relationship with liver steatogenesis.Alkhouri et al. [10] assessed the non-HDL-C levels in children with NAFLD and found that non-HDL-C had a positive association with histologic features of nonalcoholic steatohepatitis (NASH). Corey et al. [11] found that in patients who were free of lipid lowering agents, NASH was associated with significantly higher levels of non-HDL-C and concluded that non-HDL-C could be utilized as a non-invasive marker to distinguish between steatosis and NASH.Du et al. [7] found that in NAFLD patients with high TG level, non-HDL-C was better at identifying risk for NAFLD than LDL-C. This was similar to our finding. Therefore, we hypothesized that non-HDL-C has the toxic effects on the liver.
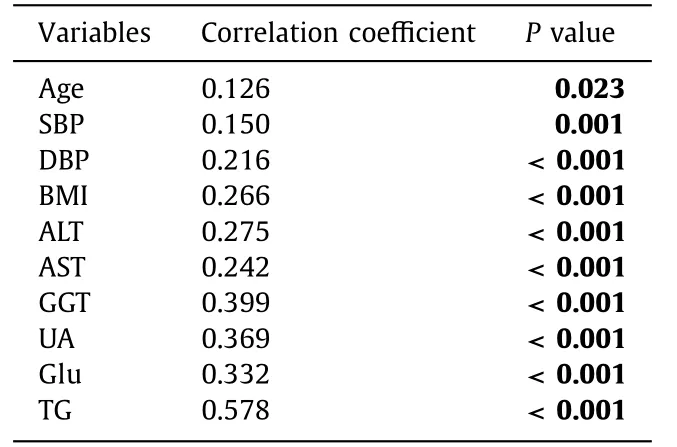
Table 2 The correlation between serum non-HDL-C level and baseline/laboratory variables in NAFLD patients.
There are some limitations in our study. Firstly, it is a crosssectional observational study that limited the definitive causality or temporal association between non-HDL-C and NAFLD. Secondly,the NAFLD diagnosis was only based on ultrasonography. Although ultrasonography has been widely used in epidemiological studies of NAFLD, it is not sufficiently sensitive to the diagnosis of mild steatosis. Thirdly, this is a single-center study. Our findings need to be validated by multicenter studies.
In summary, the detection of non-HDL-C level in NAFLD patients is of great significance. Non-HDL-C level is an important risk factor for NAFLD, which may be associated with CVD and toxic effects of excessive cholesterol on the liver.
Acknowledgments
None.
CRediT authorship contribution statement
Si-Yu Shao:Data curation, Investigation, Writing - original draft.Yi-Lan Wang:Data curation, Writing - original draft.Li-Min Feng:Formal analysis, Investigation, Methodology.Ying Zhao:Conceptualization, Funding acquisition, Project administration, Resources,Supervision, Writing - review & editing.
Funding
This study was supported by a grant from Zhejiang Natural Science Foundation ( LY20H20 0 0 025 ).
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Zhejiang University School of Medicine (No.2019-1486).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2020年6期
Hepatobiliary & Pancreatic Diseases International2020年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Non-operative management of pancreatic trauma in adults
- Increased CMTM4 mRNA expression predicts a poor prognosis in patients with hepatocellular carcinoma
- Folfirinox chemotherapy prolongs stent patency in patients with malignant biliary obstruction due to unresectable pancreatic cancer
- Role of phosphorylated Smad3 signal components in intraductal papillary mucinous neoplasm of pancreas ?
- Diagnostic accuracy of administrative database for bile duct cancer by ICD-10 code in a tertiary institute in Korea
- Long noncoding RNA HAND2-AS1 re duce d the viability of hepatocellular carcinoma via targeting microRNA-300/SOCS5 axis
