Advanced delivery strategies facilitating oral absorption of heparins
School of Pharmacy,Nantong University,19 Qixiu Road,Nantong 226001,China
Keywords:Heparins Oral delivery Multiple obstacles Stability Intestinal epithelia permeability Lymphatic transport
ABSTRACT Heparins show great anticoagulant effect with few side effects,and are administered by subcutaneous or intravenous route in clinics.To improve patient compliance,oral administration is an alternative route.Nonetheless,oral administration of heparins still faces enormous challenges due to the multiple obstacles.This review briefly analyzes a series of barriers ranging from poorly physicochemical properties of heparins,to harsh biological barriers including gastrointestinal degradation and pre-systemic metabolism.Moreover,several approaches have been developed to overcome these obstacles,such as improving stability of heparins in the gastrointestinal tract,enhancing the intestinal epithelia permeability and facilitating lymphatic delivery of heparins.Overall,this review aims to provide insights concerning advanced delivery strategies facilitating oral absorption of heparins.
1.Introduction
Venous thromboembolism (VTE) is recognized as a high death rate complication among surgery patients.Without therapy,these patients have 50%chance of catching recurrent thromboembolism,including deep-vein thrombosis(DVT)and pulmonary embolism (PE) [1,2].Given the prevalence and consequence of thrombosis,surgery patients are usually received anticoagulants treatment to prevent VTE.
The coagulation cascade is triggered by tissue factor(TF) release from vascular injury (Fig.1) [3].Anticoagulants prevent or reduce coagulation of blood by interfering with the normal function of TFs.To date,there are three kinds of anticoagulants used in the clinic[4].Different anticoagulants have different biological mechanisms to inhibit formation of VTE.The first anticoagulant is vitamin K antagonists(VKA),for example,warfarins,they inhibit coagulation by keeping prothrombin,clotting factors VII,IX and X inactive[5].These drugs have slow onset,and are subjected to low therapeutic efficacy and high drug-drug interactions[6].Therefore,they are gradually replaced by new emerging anticoagulants,namely direct oral anticoagulants (DOACs)and heparins,which show higher therapeutic efficacy than VKA.DOACs including dabigatran,rivaroxaban,apixaban and edoxaban treat VTE by targeting factor Xa (FXa) or thrombin [7,8].Although these DOACs are being used for treating VTE,life-threatening bleeding still seriously restrictstheir clinical practice [6,9–11].In order to address the risk of bleeding,a more rapid and thorough antidote may be required.Unfortunately,only one approved antidote is specific for dabigatran,no available antidotes for other DOACs,which further reduces their therapeutic potential in clinic[12].

Table 1–Summary of UFH,LMWH and synthetic pentasaccharides characteristics.

Fig.1–Schematic of blood coagulation processes(Adapted with permission from[3].Copyright 2015 Taylor&Francis).There are two processes that can initiate clotting.One is a very rapid process called extrinsic pathway,and the other one is a slower but larger intrinsic pathway.The extrinsic pathway is triggered when complex of TF(tissue factor)and factor VIIa activates factor IX and/or X.The intrinsic pathway is initiated by activation of factor XII by certain negatively charged surfaces,then the factor XIIa catalyzes the conversion of factor XI to factor XIa,and factor XIa further activates factor IX to factor IXa.
Heparins,the major anticoagulants,have over 100 years of clinical experience.In contrast with VKA,heparins have low potential of drug-drug interaction.Compared with DOACs,heparins show not only identical anticoagulation effect,but also low bleeding complication [9,10].Hence,they remain the very important anticoagulants in current clinical use.On the basis of different preparation processes,heparins can be divided into unfractionated heparin (UFH),low molecular weight heparin(LMWH)and synthetic pentasaccharides,and their main characteristics are summarized in Table 1 [13–21].Structures of UFH,LMWH and synthetic pentasaccharides are shown in Fig.2.Heparins achieve anticoagulation function primarily by binding to antithrombin III (ATIII) via a unique pentasaccharide motif [22].Once heparins bind to ATIII,they can readily dissociate and bind to additional ATIII,providing a lasting anticoagulant effect.UFH naturally existed in our bodies and its molecular weight ranges from 3000 Da to more than 30 000 Da [23].For medicinal usage UFH is extracted from bovine lung or porcine intestines.LMWH is produced by extracting the UFH and then depolymerizing it by chemical or enzymatic methods.In general,the average molecular weight of LMWH is less than 8000 Da.LMWH has a longer halflife than UFHin vivo.Synthetic pentasaccharides including fondaparinux and idraparinux,are designed by mimicking the site of UFH and LMWH that bind to the ATIII.They are homogeneous with molecular weight of 1727 Da and have the longest half-life,at least 17 h.Therefore,in comparison with UFH and LMWH,synthetic pentasaccharides could reduce the administration frequency to some extent.Heparins are essentially administered once or twice daily in clinics by subcutaneous or intravenous injection [24,25].Apparently,oral administration offers increased patient compliance and has significant clinical value to prevent VTE in a long-term chronic treatment in contrast with injection route.
The current review briefly analyzes various challenges encountered for oral delivery of heparins,and highlights several advanced delivery strategies to improve oral absorption of heparins.

Fig.2–Chemical structures of UFH,LMWH and synthetic heparins.Different heparins have different molecular weight(Mw),and the value of m+n is also various.The Mw of UFH ranges from 3000 to 30 000 Da,LMWH is about one third of the Mw of UFH.For fondaparinux and idraparinux,they are chemically synthesized and consist of just the AT III binding pentasaccharide sequence of UFH and LMWH.
2.Challenges for oral delivery of heparins
2.1.Physicochemical properties of heparins
As we know,oral drug absorption is a complex process affected by drug’s basic physicochemical properties including solubility,pKa,logP,stability and molecular weight,and any of them can influence the absorption of drug [26,27].In general,a drug that is more lipophilic may increase permeability,but may result in lower solubility,thereby decreasing oral absorption.On the other hand,a drug that is more hydrophilic may increase solubility,but may reduce the ability of drug to transport across the lipophilic intestinal epithelial cellular membrane,resulting in low oral absorption likewise[28].Drug with appropriate solubility,pKa and logP would be more likely to possess desirable oral bioavailability.
Apart from above-discussed parameters,drug molecular weight also determines absorption.According to Lipinski’s rule of five [29],to be a good candidate for oral absorption,the molecular weight of the drug has to be less than 500 Da.The molecular weight of heparins is over that.What’s more,heparins are hydrophilic macromolecules with high-density negative charges.Altogether,the poor physicochemical properties make free heparins almost cannot pass through gastrointestinal tract into systemic circulation.
2.2.Biological barriers for heparins
When administered by oral route,drugs go through following steps to enter into systemic circulation.Drugs first go to stomach via esophagus,then to the small intestine,where drugs are absorbed into portal vein or lymphatic capillaries,and carried to the liver or lymphatic system,and finally to systemic circulation.During the entire transport process,several major barriers impede oral delivery of heparins.The first biological barrier is the hash acidic conditions in the stomach.After exposure to gastric acid,heparins are easily degraded,leading to drug activity loss [30,31].Mucus layer is the second biological barrier.The entire gastrointestinal tract is lined by mucus layer,which is composed of water and negatively charged mucin molecules [32].The mucus is responsible for capture and elimination of foreign moieties,impeding their contact with the underlying intestinal epithelial layer.In addition to mucus layer,intestinal epithelial cells act as a barrier to prevent exogenous harmful substances including foreign antigens,microorganisms and toxins,from crossing into systemic circulation [33–35].Some essential nutrients,electrolytes and water can be absorbed into blood circulation through transepithelial/transcellular and paracellular pathways.Transcellular permeability is selectively regulated by special transporters for amino acids,fatty acids,sugar and electrolytes [36,37].For heparins,there is no exclusive transporter in the intestinal epithelial cells.Paracellular permeability is regulated by intercellular complexes localized at apical membrane junction.The average pore size of tight junction in the intestine is approximately 3–9 ?A,and related data suggested that molecules with a size over 15 ?A (about 3.5 kDa) cannot be transported through this route [38].Heparins are regarded as exogenous substance after oral administration,and their molecular sizes are larger than the pore size of tight junctions,except for synthetic pentasaccharides.Under normal circumstance,it’s quite difficult for heparins to pass through the intestinal epithelial cells.Even if heparins are absorbed into intestinal epithelial cells,their possible intracellular trafficking from endosome to lysosome is another barrier[39].Lysosome maintains acidic environment and contains large amounts of hydrolytic enzymes that may cause loss of drug activity.
Basically,drug travels to the liver through hepatic portal vein after drug leaving intestine.There are many kinds of enzymes for drug metabolism in the liver.Heparinase,one of them,can induce degradation of heparins [40].Finally,hepatic metabolism leads to reducing the oral bioavailability of heparins.Together,multiple biological barriers seriously hinder the heparins absorption into systemic circulation.
3.Strategies for oral delivery of heparins

Fig.3–The chemical structures of several kind of typical pH-sensitive polymers used for oral delivery of heparins.(A)Acrylic-based polymers;(B)hydroxypropyl methylcellulose phthalate(HPMCP)and hydroxypropyl methylcellulose acetate succinate(HPMCAS);(C)alginate.
In spite of the above-mentioned physicochemical and biological barriers for heparins,advanced delivery strategies,like prodrug and nanoparticles/microparticles can be adopted to overcome these barriers and improve the oral delivery of heparins.And,these delivery carriers can act as combined multifunctional tools to address these problems as follows:(1) improve stability of heparin in the gastrointestinal tract;(2) enhance the intestinal epithelial cell permeability; (3)facilitate lymphatic transport of heparins.
3.1.Improve stability of heparins in the gastrointestinal tract
The good stability of heparins in gastrointestinal tract is a basic precondition for achieving excellent oral absorption.Considering that heparins are unstable in the stomach,they can be loaded into oral pH-sensitive drug delivery systems to improve the stability in the gastrointestinal tract[41–44].For these pH-sensitive delivery systems,they can preserve their structures in the stomach(pH ≈2),and release heparins in the intestine (pH ≈7),which protects heparins from acid degradation at stomach.These oral pH-sensitive delivery systems are usually constructed by pH-sensitive polymers,including acrylic-based polymers,hydroxypropyl methylcellulose derivatives and sodium alginate.Their main chemical structures can be summarized in Fig.3.
Acrylic-based polymers such as EudragitR○polymers are extensively used to fabricate pH-sensitive drug delivery system.Nanoparticles or microparticles established by these polymers retain a collapsed state in the low pH of stomach due to the protonation of carboxyl groups (-COOH).After gastric passage,an increase in pH leads to nanoparticles or microparticles swelling due to carboxyl ionization and hydrogen bond breakage.For example,EudragitR○P4135F polymer [45],heparins released from Eudragit P4135F microspheres not over 20%at pH<6,so most of heparins can avoid acid degradation and maintain active before reaching to intestine.
In addition to EudragitR○polymers,some hydroxypropyl methylcellulosederivativesincludinghydroxypropyl methylcellulose phthalate (HPMCP) and hydroxypropyl methylcellulose acetate succinate (HPMCAS) are applied to prepare pH-sensitive drug delivery system.This type of polymers is insoluble at low pH and soluble (ionized) at intestinal pH.HPMCP-modified nanoparticles could reduce heparin premature release in the stomach and release the heparin in the intestine.The oral absolute bioavailability of heparin in HPMCP-modified nanoparticles was 2.5-fold higher than in pure nanoparticles[46].
Sodium alginate is another kind of natural polymer that has been exploited for oral delivery of heparins without risk of mucosal damage.Sodium alginate is assigned to a serious of natural unbranched polyanionic polysaccharides ofβ-D-mannuronic acid (M) andα-L-guluronic acid (G)repeating units linked by a 1→4 linkage.Because of carboxyl groups,sodium alginate is protonated into insoluble form of alginic acid and exhibits low swelling ratio under acidic conditions,but tend to increase the swelling behaviors under basic condition.Archana et al.[47] developed alginate coated chitosan core shell nanoparticles for oral delivery of LMWH,and alginate coated chitosan nanoparticles not only decreased release rate of LMWH in the acidic pH,but also shown 3-fold increase in oral bioavailability in comparison with LMWH solution.
3.2.Enhance the intestinal epithelia permeability
As shown in Fig.4,drugs transport across intestinal epithelia cells mainly through following three ways [48,49].The efficiency of each transport way depends mostly on the drug’s basic physicochemical properties,such as molecular weight,hydrophobicity,ionization degree [50,51].Absorption enhancement across the intestinal epithelial cells can be achieved by different delivery systems.Heparins associated with formulation and delivery system can pass through cells via different mechanisms including:(1) enhancing lipophilicity of heparins to improve transcellular absorption;(2) targeting to intestinal epithelia special receptors or transporters to increase transcellular absorption; (3) using absorption enhancers to facilitate transcellular or paracellular absorption.

Fig.4–Schematic representation of drug transport pathways across intestinal epithelial cells.(a)Transcellular transport by passive diffusion;(b)transcellular transport mediated by special receptor or transporter;(c)paracellular transport by opening tight junction.
3.2.1.Enhancing lipophilicity of heparins
Intestinal epithelial cellular membrane is a phospholipid bilayer structure.However,heparins are hydrophilic molecules.Therefore,they cannot be directly absorbed through intestinal epithelial cells by passive diffusion.Different lipids from plants or animals including triglycerides,steroids and phospholipids could be utilized to enhance the lipophilicity of heparins,which are generally safe for human health.In such a strategy,lipids were usually used in combination with nanoparticles to integrate the advantage of both.For one thing,nanoparticles carrying drug can be ingested through adsorptive endocytosis processes by intestinal epithelial cells.For another thing,lipids help to increase the interaction between nanoparticles and intestinal epithelial membrane,facilitating oral absorption.
The group of Mao [52–54] has tried to use fatty glycerides with different chain length to enhance the lipophilicity of LMWH-loaded nanoparticles.The influence of glyceride chain length (short-chain,medium-chain and long-chain fatty acids) on oral absorption was investigated.It was found that all tested fatty glycerides modified-nanoparticles could improve oral bioavailability of LMWH,and short-chain fatty acid performed better absorption enhancement.In recent study [55],this group also studied the influence of fatty glycerides amount on hydrophobicity of nanoparticles and oral absorption of LMWH.The results showed that all tested amount of fatty glycerides could not only enhance the hydrophobicity of nanoparticles,but also improve oral absorption of LMWH.Apart from fatty glycerides,squalene,a natural lipid,was also exploited to enhance the lipophilicity of fondaparinux.Cationic squalene derivates are synthesized,and then mixed with anionic fondaparinux to form nanoparticles.Thein vivopharmacokinetic study showed that the oral absorption of fondaparinux was increased[56].
3.2.2.Targeting to intestinal epithelia receptor/transporter
As stated earlier,the small intestine plays a critical role in the absorption of drugs,nutrients and many other molecules.In addition,the intestine is equipped with specialized cell membrane-bound transporters,receptors and transport mechanisms [49].Thus,modifying drugs or drugs-loaded nanoparticles by coupling a special targeting molecule could be an efficient way to enhance the intestinal epithelial cell permeability of drugs.Some investigators have used the targeting ligands such as folic acid[57,58],vitamin B12[59–62],transferring[63–65],lectins[66,67]to facilitate macromolecule drugs absorption.In this way,the affinity between drugs or drugs-loaded nanoparticles and intestinal epithelial cells is strengthened.
A lot of attempts have been made by the group of Youngro Byun [68–72] to design bile acid-modified nanoparticle to improve the trans-membrane ability of heparins.Bile acids are bio-inspired and bio-mimetic small molecules that are secreted from the liver.Their chemical structures are shown in Fig.5A.Basically,bile acids conjugate with heparins via amide bond.In order to keep bioactivity of heparins,AT III binding pentasaccharide sequence is always not selected to be a bind site.Theoretically,bile acids are supposed to be absorbed by apical sodium-dependent bile acid transporters(ASBT)which is over expressed in the ileal[73].ASBT mediate the endocytosis of bile acids-modified nanoparticles across the ileal enterocyte apical membrane.After entering the cytoplasm,the nanoparticles bind to the ileal bile acid binding protein (IBABP) and then are carried in the form of vesicles to transporter in the basolateral membrane.As a consequence,nanoparticles are transported into blood circulation by exocytosis(Fig.5B)[74].
In comparison with other targeting molecules,bile acids offer the advantage of avoiding to fuse with endosome/lysosome [75],so that nanoparticles could retain their intact morphological structures,which protects heparins from acid degradation before entering into blood circulation.In addition,bile acids-modified nanoparticles could transport through enterocytes,which maximums the advantage of nanoparticles and facilitates heparins absorption.Thus,targeting to intestinal epithelia receptor,especially ASBT,is a very promising way to improve oral absorption of heparins.These targeting molecules such as bile acids not only enhance uptake of heparins,but also facilitate lysosomes escape and exocytosis of heparins,leading to absorption enhancement.
3.2.3.Absorption enhancers
Absorption enhancers are functional excipients to improve the absorption of active drug.For oral delivery of heparins,absorption enhancers refer to an agent whose function is to increase intestinal epithelial membrane permeability,sometimes they are also specifically called permeability enhancers [76].These include a series of natural,synthetic and semi-synthetic substances,such as surfactants[77],EDTA[78],chitosan and chitosan derivatives[79–82].The commonly used absorption enhancers for heparins are shown in Table 2[83–93].The possible mechanisms of absorption enhancers to improve heparins intestinal transport include opening tight junctions,or increasing membrane permeability or a combination of both.Absorption enhancers play their roles usually in free forms,but they can simply mix with heparins or load into a formulation before administration.

Fig.5–(A)Basic chemical structures of bile acids(BA);(B)schematic representation of transport process for BA modified heparins.

Table 2–Examples of absorption enhancers tested in oral delivery of heparins.

Fig.6–Illustration of some strategies utilized to improve drug loading into lipid-based nanocarriers.(a)Hydrophilic heparins are conjugated with hydrophobic molecules to enhance lipophilicity;(b)hydrophilic heparins mix with hydrophobic positive molecules through electrostatic interaction to enhance lipophilicity;(c)hydrophilic heparins firstly loaded into a W/O/W emulsion and then the hydrophobic emulsion loaded into lipid carriers;(d)hydrophilic heparins firstly loaded into a reverse micelle and then loaded into lipid carriers.
The EligenR○ carrier (Sodium N-[8-(2-hydroxybenzoyl)Amino] caprylate (SNAC) is cationic cell-penetrating peptide,a number of related researches indicated that SNAC has markedly increased the gastrointestinal absorption of heparins [94],and clinical studies suggested that SNAC can guarantee therapeutic levels of heparins [95].SNAC enables heparins transport across intestinal epithelia cells via the transcellular pathway.Other absorption enhancers such as cationic polymers are also extensively used to boost the absorption of heparins.They accomplish absorption enhancement largely via opening the tight junction.
3.3.Facilitate lymphatic delivery of heparins
Physiologically,the lymphatic system acts as an important role in fluid homeostasis,lipid metabolism and immune control [96].For oral delivery of heparins,there are two ways to facilitate lymphatic transport.One approach is to enhance the lipophilicity of drugs and then combine with lipid carriers.Lipophilic drugs loaded lipid carriers can be synthesized to form chylomicrons and enter into lymphatic system[97–99].Yet another approaches to load the drugs into a carrier and the drug-carrier may be absorbed by special intestinal cells such as M cells (Peyer’s patches) [100].It has been reported that lipid carriers with appropriate size and shape can be selectively ingulfed by M cells[101].Excellent indepth reviews about lymphatic transport pathway have been published elsewhere [102–104].To improve drugs especially highly lipophilic drugs lymphatic transport,lipids,particularly long chain fatty acids,have been frequently utilized to enhance the lymphatic absorption of drugs[105].Heparins are hydrophilic macromolecules,in order to facilitate lymphatic delivery,it’s quite crucial to enhance the lipophilicity of heparins by conjugation of lipid molecules,and then lipophilic conjugates are encapsulated into lipid carriers.In addition,some strategies can be taken to improve the drug loading into lipid carriers,and then these heparins-loaded lipid carriers are transported into lymphatic system via M cells.Therefore,lipid-based nanocarriers have been widely applied to facilitate lymphatic transport.
In the following section,three kinds of lipid carriers reported to delivery heparins will be discussed in detail.They are solid lipid nanoparticles,microemulsions and lipid nanocapsules.Fig.6 shows all the methods developed to enhance the drug loading capacity into lipid-based nanocarriers.
3.3.1.Solid lipid nanoparticles
Solid lipid nanoparticles (SLNs) composed of solid lipids (at room temperature) have been attracted increasing attention for oral delivery of drugs during recent years [106–108].For hydrophilic heparins,direct incorporation into SLNs will result in very low encapsulation efficiency and drug loading.Paliwal et al.[109] have used saturated fatty acid lipids with varying chain length to conjugate with LMWH to improve lipophilicity.Lipidation of LMWH not only ensured higher encapsulation efficiency and drug loading within SLNs,but also made them suitable for lymphatic transport.In vivostudy demonstrated that the maximum anti-FXa activity of these developed LMWH-loaded SLNs is almost double that of free LMWH.
3.3.2.Microemulsion
Microemulsions are clear,thermodynamically stable,isotropic liquid mixtures of oil,water and surfactant,frequently in combination with a cosurfactant [110].Similarly,to ensure the drug loading and encapsulation efficiency of LMWH,Kim et al.[111] have synthesized conjugates of LMWH and deoxycholic acid (DOCA) and then encapsulated the conjugates into a microemulsion system.Simple LMWHDOCA conjugates could not significantly change the oral absorption of LMWH.But for LMWH-DOCA in microemulsion,its oral bioavailability is increased up to 1.5%.One of the most important mechanisms is that microemulsion could carry lipophilic LMWH-DOCA conjugates getting into the lymphatic system,and circumvent first pass metabolism in the liver.
3.3.3.Lipid nanocapsules
Lipid nanocapsules (LNCs) is a hybrid carrier between polymeric nanocapsules and liposomes,which combined the advantages of colloidal particles and lipid carriers [112].LNCs are prepared based on a solvent-free phase-inversion temperature process with a size of about 100 nm.It has been reported that LNCs could transport across intestinal epithelium via transcellular pathway and remain their original intact nanoparticles structure after exocytosis [113].For most small molecule drugs delivered orally,transport from intestinal interstitial space occurs primarily via the blood capillaries because blood flow rate in these vessels are~100–500-fold higher than lymph flow [97].By contrast,nanocarriers are prone to penetrate the lymphatics because their sizes are too large to get through blood capillaries,but lymphatics are not continuous [99,114].Therefore,when LNCs enter into intestinal interstitial space,LNCs would preferably leak into lymphatics to avoid hepatic metabolism.Ramadan et al.[115]have developed two cationic surfactant-coated lipid nanocapsules (cLNCs) for loading negatively-charged fondaparinux.The fondaparinux-loaded cLNCs show significant enhancement in oral absorption and bioavailability.
4.Future perspective
Achieving efficient and effective heparins delivery via oral route is meaningful due to its simplicity and acceptability.In spite of multiple barriers before absorption into systemic circulation,advanced delivery strategies have been employed for oral delivery of heparins,including protection of drug in the gastrointestinal (GI) tract environment,enhancing intestinal epithelial cell permeability of drug,and facilitating lymphatic transport of drug.Any above-mentioned single strategy could improve oral absorption of heparins to some extent.Of note,simply improving the GI stability of heparins is not enough to ensure pretty good bioavailability,since the heparins cannot transport across the intestinal epithelial cells.Under such a condition,the fabricated delivery systems combination of increasing GI stability and intestinal permeability of heparins would provide better oral absorption than single one.The delivery systems that could facilitate lymphatic transport of heparins suggest they improve intestinal permeability of heparins simultaneously,because heparins should transport through intestinal epithelia before entry into the lymphatic system.It seems that the strategy that facilitates lymphatic transport hold more advantages since it can overcome more barriers.
Theoretically,an ideal delivery system should address all the hurdles encountered during the entire absorption process.To integrate all these functions in one formulation,the constructed delivery systems are usually is complex.Thus,one important challenge for designing these ideal delivery systems is to maintain the simplicity in the formulation.With the development of materials engineering,it’s still prospective to develop newly multifunctional all-in-one excipients to overcome all obstacles.
5.Conclusion
In summary,the development of oral formulation or delivery carrier for heparins will avoid the inconvenience of parental administration.And the advanced delivery systems show fantastic advantages that they are able to bypass certain barriers during oral absorption.In contrast with free heparin solutions,single formulation and delivery strategy indeed can significantly improve oral absorption of heparins.To maximum the effects of delivery strategies for heparins,two crucial points probably need to be addressed when researchers design oral delivery systems for heparins:(1)integrate strategies covering several advantages into one carrier;(2)make sure that ATIII binding site of heparins is not be damaged.Above all,designing reasonable delivery systems is rather essential for oral delivery of heparins in the near future.
Conflicts of interest
The authors report no conflicts of interest.The authors alone are responsible for the content and writing of this article.
Acknowledgments
This work was supported by the Natural Science Fund for Colleges and Universities in Jiangsu Province (No.18KJB350009),the Natural Science Fund for Colleges and Universities in Jiangsu Province (No.17KJB350009) and the Natural Science Foundation of Jiangsu Province (No.BK20170445).
Supplementary materials
Supplementary material associated with this article can be found,in the online version,at doi:10.1016/j.ajps.2019.11.006.
 Asian Journal of Pharmacentical Sciences2020年4期
Asian Journal of Pharmacentical Sciences2020年4期
- Asian Journal of Pharmacentical Sciences的其它文章
- Enhancement of oral bioavailability and anti-Parkinsonian efficacy of resveratrol through a nanocrystal formulation
- Fluidised bed granulation of two APIs:QbD approach and development of a NIR in-line monitoring method
- Quantitative prediction of the bitterness of atomoxetine hydrochloride and taste-masked using hydroxypropyl-β-cyclodextrin:A biosensor evaluation and interaction study
- In situ apolipoprotein E-enriched corona guides dihydroartemisinin-decorating nanoparticles towards LDLr-mediated tumor-homing chemotherapy
- Let-7 miRNA and CDK4 siRNA co-encapsulated in Herceptin-conjugated liposome for breast cancer stem cells
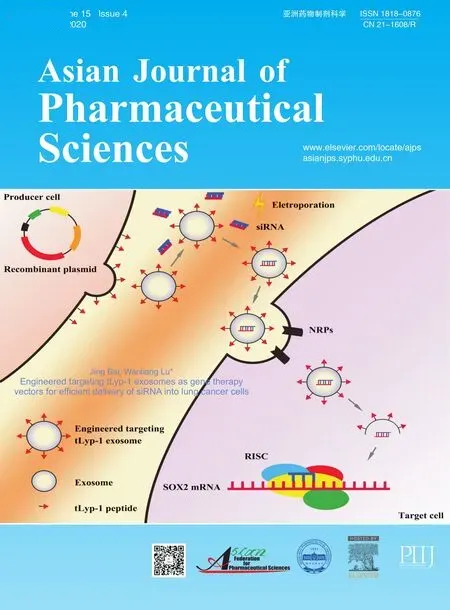
- Engineered targeting tLyp-1 exosomes as gene therapy vectors for efficient delivery of siRNA into lung cancer cells
