Robotic gastrectomy for gastric cancer
Masanori Tokunaga, Masahiro Watanabe, Shizuki Sugita, Akiko Tonouchi, Akio Kaito, Takahiro Kinoshita
Gastric Cancer Division, National Cancer Center Hospital East, Kashiwa 277-8577, Japan.
Abstract Robotic gastrectomy (RG) is increasingly performed, particularly in East Asia. With articulated devices, surgeons are able to perform every procedure more comfortably and meticulously, which makes RG ideal from the surgeon’s standpoint.However, it is still unclear whether it is a suitable treatment strategy from the patient’s viewpoint, due to the lack of solid evidence obtained from randomized controlled trials. The feasibility of RG has been demonstrated in many retrospective comparative studies, which showed similar trends, including relatively less estimated blood loss and longer operation time with RG than laparoscopic gastrectomy (LG), equivalent number of harvested lymph nodes and similar length of postoperative hospital stay between RG and LG. However, considering the higher medical expenses associated with RG,its superiority in terms of long-term survival outcomes will need to be confirmed for it to be accepted more widely.
Keywords: da Vinci, robot, gastric cancer, robot assisted gastrectomy, laparoscopic gastrectomy
INTRODUCTION
Minimally invasive surgery (MIS) for gastric cancer has been increasingly performed in the East, where incidence of the disease is high and approximately half of cases are diagnosed at an early stage[1-3]. The non-inferiority of laparoscopic gastrectomy (LG) for early gastric cancer comparing to open gastrectomy in terms of short- and/or long-term outcomes has been confirmed by randomized controlled trials, and that for advanced gastric cancer is under investigation and may be shown in the near future[4-7]. However, LG has several shortcomings which include limitation in the movement range of forceps and the two-dimensional surgical view available to operating surgeons, and it will be necessary to overcome these issues for MIS to be accepted more widely.

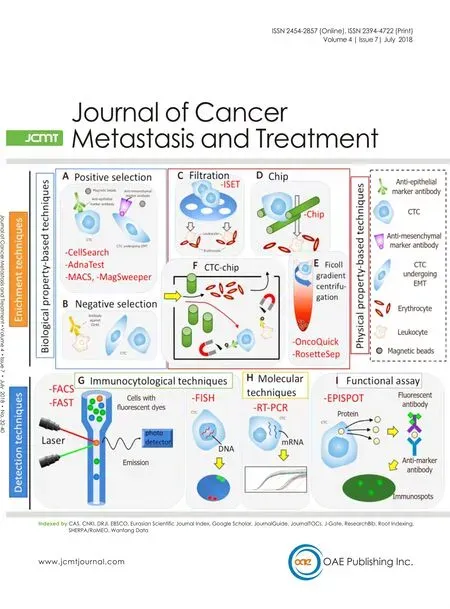
Figure 1. (A) Surgical field during LG: straight devices without articulation are used; (B) surgical field during RG: articulated devices are used
Using the da Vinci? Surgical System (Intuitive Surgical, Sunnyvale, CA, USA), a system for robotic surgery,surgeons are able to attain a three-dimensional view, instrumentflexibility, tremor suppression, and improved ergonomics, which are thought to be advantages of robotic gastrectomy (RG)[8-11]. With these advantages,theoretically, RG enables surgeons to perform more precise surgery with less trauma, which could result in superior outcomes over LG. However, the number of comparative prospective studies between RG and LG is quite limited, and therefore, solid evidence supporting RG does not yet exist[12-16].
Herein, we would review the comparative retrospective and prospective studies which have investigated the differences in short- and long-term surgical outcomes between RG and LG.
Clear advantages of RG over LG
There are several clear benefits of RG which contribute to reducing invasiveness and trauma compared with LG. Articulated devices, which are only available in RG, make each surgical technique more meticulous and precise, and are thought to be one definitive advantage of RG [Figure 1][8-13]. Other apparent advantages include a tremor suppression function, which is helpful to keep a stable surgicalfield and effective to reduce organ injury, and a three-dimensional image, which has become available in LG although special equipment is necessary. With these clear advantages, RG is expected to have advantages over LG. Clear and possible advantages and disadvantages of both procedures are summarized in Table 1.
Clear disadvantages of RG
Because RG requires expensive machines and devices, cost effectiveness is an intriguing issue for surgeons,and seems to be an absolute disadvantage of RG. In Korea and Japan, where more than half of reports havebeen published, the cost for RG is not yet reimbursed by government, and therefore patients or hospitals have to pay additional fees[17]. In contrast, medical expense for LG is partially covered by national insurance systems, and the cost burden on patients and hospitals is obviously less than for RG. The additional fee for RG differs between surgeries depending on how many disposable and re-usable instruments are used.Previously, some comparative studies investigated the difference in medical expense between RG and LG and reported that RG expenses were approximately twice as great[18-21]. In a prospective comparative study conducted in Korea, significantly higher total cost in the RG group (US$13,432) than the LG group (US$8090)was also reported[14]. However, if medical expenses associated with RG decrease in the future, they will no longer be an absolute disadvantage of RG.

Table 1. Advantages and disadvantages of RG vs. LG are summarized
COMPARISON OF SHORT-TERM SURGICAL OUTCOMES BETWEEN RG AND LG
Short-term surgical outcomes between RG and LG have been compared in many retrospective and a few prospective studies[9,14-20,22-44]. Among short-term surgical outcomes, intraoperative blood loss, the duration of surgery, the number of retrieved lymph nodes, the incidence of postoperative complications, and the length of postoperative hospital stay are thought to reflect surgical quality, and were assessed in most studies.
Intraoperative blood loss was generally equivalent or less during RG than LG [Table 2]. The magnifiedfine three-dimensional view attained in RG enables surgeons to recognize even very small vessels, and with articulated devices, they can surely stanch bleeding. However, the reported statistically significant differences in intraoperative bleeding between LG and RG were generally less than 100 mL except for one report from Korea[38], and it is unclear whether the difference is clinically significant of not. Statistically significant more blood loss in RG was also reported in two Japanese studies, but the differences were less than 20 mL[33,41].
The duration of surgery is significantly longer in RG than in LG in all report, and the difference was statistically significant in most series [Table 3]. Although the difference ranged from 14 to 124 min, it took RG generally approximately 60 min more operation time than LG. There are several probable explanations for longer operation time in RG. Firstly, it takes 15 to 30 min, known as docking time, to prepare before an operator begins the surgery at a console. Secondly, during RG, a surgeon uses four robotic arms, which is less than the average number offive ports used during conventional LG. Although an additional port for an assistant can be used in RG, it is under the assistant’s not the surgeon’s control, and is sometimes useless due to collisions with robotic arms. As a result, it becomes difficult to make afine surgicalfield, particularly in patients with high visceral fat volume or advanced disease, and therefore might cause longer operation time.
The number of retrieved lymph nodes was reported to be almost equal between RG and LG. The duration of postoperative hospital stay was also similar, although a few investigators reported that it was shorter following RG than LG.

Table 2. Comparison of blood loss
The incidence of postoperative complication was compared between the approaches [Table 4]. Many investigators have thought that RG could be safer than LG, because articulated devices, the three-dimensional image, and the tremor suppression function could make recognition of anatomical structures much easier and lymphadenectomy much safer. However, unexpectedly, significantly lower morbidity rate was reported only in two reports, and the difference, even if morbidity rate was lower in RG than LG, was not statistically significant in other reports[33,41]. Considering the current status of LG, which is already a well-established safe procedure, it seems to be very difficult to show that RG could further improve the safety. Mortality rate was not statistically significant between RG and LG in any of the studies, and therefore, both RG and LG seem to be safe procedures in terms of postoperative morbidities and mortality.
Long-term outcomes between RG and LG
The number of reports focusing on long-term survival outcome is quite limited [Table 5]. Three Korean series,which were from a single institute with different study populations, and one Japanese series, reported longterm outcomes with a median follow up period of at least three years[32,33,35,40]. In the Korean series, Lee et al.[32]focused on patients undergoing D2 distal gastrectomy, Son et al.[39]included patients undergoing spleen-preserving total gastrectomy, and Okumura et al.[34]compared long-term survival outcomes of elderly (70 years old or older) patients between RG and LG. None of these studies showed significant survival differences.The Japanese series by Nakauchi et al.[17]compared three-year overall and recurrence free survival between RG and LG, and reported that no statistically significant difference was found even after stratification by pathological stage. However, the lack of the results of prospective comparative studies focusing on longterm survival makes it difficult to obtain any conclusive result in terms of long-term survival outcomes.Considering the total medical expense of RG, long-term outcomes of RG need to be better than those of LG,and should be confirmed by future prospective trials.

Table 3. Comparison of operation time
PROSPECTIVE STUDIES
Although quite a few retrospective studies already exist, the number of prospective studies, particularly that of prospective comparative studies, is extremely limited so far[12-14,16].
Kim et al.[14]reported the results of a prospective non-randomized comparative study. In their study, a total of 423 patients selected either RG or LG after they received a comprehensive explanation of each procedure, and were matched according to surgeon, extent of gastric resection, and sex. Similar early surgical outcomes including morbidity and mortality rate, except for longer operation time in the RG group were reported.
The results of a single-center prospective randomized trial, in which patients were allocated to either open(n = 153) or robotic (n = 158) gastrectomy groups, were reported by Wang et al.[16]. Similar complication rates between the groups, and less estimated blood loss, longer duration of surgery, and shorter postoperative hospital stay in the robotic group than the open group were reported.

Table 4. Compararison of postoperative morbidy and mortality

Table 5. Studies which provided long-term survival outcomes
DISCUSSION
RG has several absolute advantages, which include articulated devices, tremor suppression function, and afine three-dimensional view, and surgeons can perform operations comfortably with these technologies.However, these advantages are from the surgeons’ perspective, and it is unclear whether these technologies applied to RG are also advantageous from the patients’ viewpoint. Theoretically, the more meticulous and precise surgeries are, the better the outcomes will be. However, for RG to be more widely accepted, advantages from the patients’ side should be demonstrated in clinical trials, ideally in prospective randomized trials.
Short-term surgical outcomes such as intraoperative bleeding, surgical time, duration of postoperative hospital stay, and postoperative morbidity and mortality rate are thought to reflect surgical quality, and some of them directly affect patients’ quality of life. Therefore, these factors are frequently compared between surgical procedures, when investigators need to show superiority or non-inferiority of a newly emergent procedure. Indeed, they have been compared in many studies of RG and LG. However, it seems difficult to conclude that RG is a superior procedure to LG in terms of short-term surgical outcomes, because RG is a more time-consuming procedure, but does not show any obvious benefits. Although some have reported that RG is associated with less bleeding, the differences, which were generally less than 100 mL, seem not to be clinically meaningful. It might be difficult to demonstrate that RG could further improve short-term surgical outcomes, because LG is already a well-established and satisfactorily safe procedure.
The number of studies focusing on long-term surgical outcomes is quite limited, due to insufficient follow-up period in each study. So far, similar long-term survival outcomes between RG and LG have been reported,and we need to wait for the results of currently ongoing studies to reach any conclusions about long-term survival outcomes.
Interpretation of the results of comparative studies should be done carefully because of possible selection bias. In most comparative studies, surgical approaches were selected by the patients themselves after thoughtful explanation of both procedures, but the possibility of selection bias should be taken into account.To overcome this issue, well designed prospective, hopefully randomized controlled, trials are necessary,and we have to at least wait for the results of prospective non-randomized comparative studies[14].
To demonstrate the feasibility of RG, the surgical outcomes of RG are usually compared with those of LG.However, considering that both surgeries were developed on the concept of being minimally invasive, the differences between RG and LG might be marginal, even if RG is truly a superior procedure to LG. In addition RG is, so far, obviously the more expensive surgical procedure. Therefore, it seems unrealistic for RG to completely replace LG with all surgeries in the very near future. However, if the cost of RG decreases dramatically and high medical expense is no longer a problem, it may be a different story with RG becoming further widespread.
So far, RG seems to be as feasible as LG in terms of short- and long-term surgical outcomes. However, RG is an expensive procedure at present, and it is unclear whether RG is superior to LG from the patients’standpoint. The results of well designed prospective comparative studies are awaited to obtain conclusive results on this issue.
DECLARATIONS
Authors’ contributions
Analysed and interpreted the data: Tokunaga M, Watanabe M, Sugita S, Tonouchi A, Kaito A, Kinoshita T Read and approved thefinal manuscript: Tokunaga M, Watanabe M, Sugita S, Tonouchi A, Kaito A,Kinoshita T
Availability of data and meterials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
? The Author(s) 2018.
 Journal of Cancer Metastasis and Treatment2018年7期
Journal of Cancer Metastasis and Treatment2018年7期
- Journal of Cancer Metastasis and Treatment的其它文章
- Molecular mechanism of peritoneal dissemination in gastric cancer
- AUTHOR INSTRUCTIONS
- Circulating microRNAs as a liquid biopsy: a nextgeneration clinical biomarker for diagnosis of gastric cancer
- Laparoscopic personalized function-preserving gastrectomy with sentinel node mapping for earlystage gastric cancer
- New insights into the role of intra-tumor genetic heterogeneity in carcinogenesis: identification of complex single gene variance within tumors
- Surgical treatment of stage IV gastric cancer: is it worthwhile?
