Restrictive perimembranous ventricular septal defect with left to right Shunt post urgent aortic balloon valvuloplasty and transcatheter aortic valve replacement
Emmanouil Chourdakis, Ioanna Koniari, Nicholas G Kounis, Dimitrios Velissaris, George Hahalis,Karl Eugen Hauptmann
1Cardiology Department, Hospital of the Brothers of Mercy, Trier, Germany
2Cardiology Department, Queen Elizabeth University Hospital, Birmingham, UK
3Cardiology Department, Patras University Hospital, Rio, Patras, Greece
An 86-year-old male patient was admitted in our cardiology ward with signs of congestive biventricular heart failure. The patient presented with deteriorating dyspnea on mild exertion and at rest the last days, compatible with class NYHA III-IV heart failure, bilateral peripheral oedema,increased NT-proBNP (9198 pg/mL), mildly elevated Troponin (TnT 64 pg/mL), interstitial pulmonary oedema and bilateral pleural effusions in chest X ray. Permanent atrial fibrillation, known left branch bundle block (QRS = 170 ms), hypertension, and chronic renal failure were referred as co-morbidities. The transthoracic echocardiogram (TTE)revealed severely impaired left ventricle (LV) function[ejection fraction (EF) = 25%–30%] with diffuse wall hypokinesia, a high-grade aortic stenosis with mean trans valvular pressure gradient of 44 mmHg, despite the low ejection fraction, accompanied with mild-moderate aortic regurgitation in the context of a severe degenerative tricuspid aortic valve disease, an ascending aorta aneurysm with 5.4 cm diameter, as well as severe pulmonary hypertension (85 mmHg). The patient demonstrated mild clinical improvement with intravenous diuretic therapy and given the very high surgical risk (estimated logistic Euroscore II = 41%)for aortic valve replacement, retrograde aortic balloon valvuloplasty as a bridge to transcatheter aortic valve replacement (TAVR) was decided.
The patient clinical status deteriorated significantly in the following days, presenting signs of cardiogenic shock. Emergency retrograde aortic balloon valvuloplasty was performed under general anesthesia and transoesophageal echo guidance. Due the urgent procedure, two-dimensional and threedimensional multislice CT (MSCT) was not performed. The coronary angiogram and ventriculography showed a severe impaired ejection fraction (EF = 20%) with diffuse left ventricular hypokinesia and an isolated 70% diagonal branch ostium stenosis. Invasive mean transaortic pressure gradient was 54 mmHg. Retrograde valve passage with an AL 1 and subsequent aortic valvuloplasty with an 18/40 mm and 20/40 mm Nucleus balloon was performed during rapid ventricular pacing, resulting in a mild valve gradient reduction but significant increase of aortic regurgitation. Consequently, TAVR with successful implantation of a 29 mm Edwards Sapien-3 was performed. Interestingly, a small tear and a mild shunt in the right ventricle was revealed by a small contrast extravasation during aortography at the end of the procedure (Figure 1). The transesophageal echocardiography (TOE) demonstrated a small left to right ventricular shunt due to aortic annular rupture, resulting in iatrogenic perimembranous ventricular septal defect VSD (Figures 2 & 3). The patient extubation was uneventful without other post interventional complications.
The TTE directly following TAVR reported an appropriate prosthetic valve position without evidence of obstruction or transvalvular aortic regurgitation, except a mild paravalvular aortic regurgitation due to malapposition in the aortic annulus. Furthermore, a continuous flow presence during systolic and diastolic period, with systolic predominance,via an aortic root tear ending in the right ventricle (left to right direction) was revealed. Further quantification of Qp/Qs ratio was 1, a peak gradient via tear of 75 mmHg and stable systolic pulmonary arterial pressure, rendering the shunt as restrictive after TAVR without hemodynamic significance (Figures 4 & 5).

Figure 1. A small contrast extravasation due to a small tear and a mild shunt in the RV was identified during aortography (LAO cranial) at the end of the procedure. Correct position the 29 mm Edwards Sapien-3 prosthesis, intravenous pacemaker lead in the right ventricle. LAO: left anterior oblique view; RV: right ventricular.
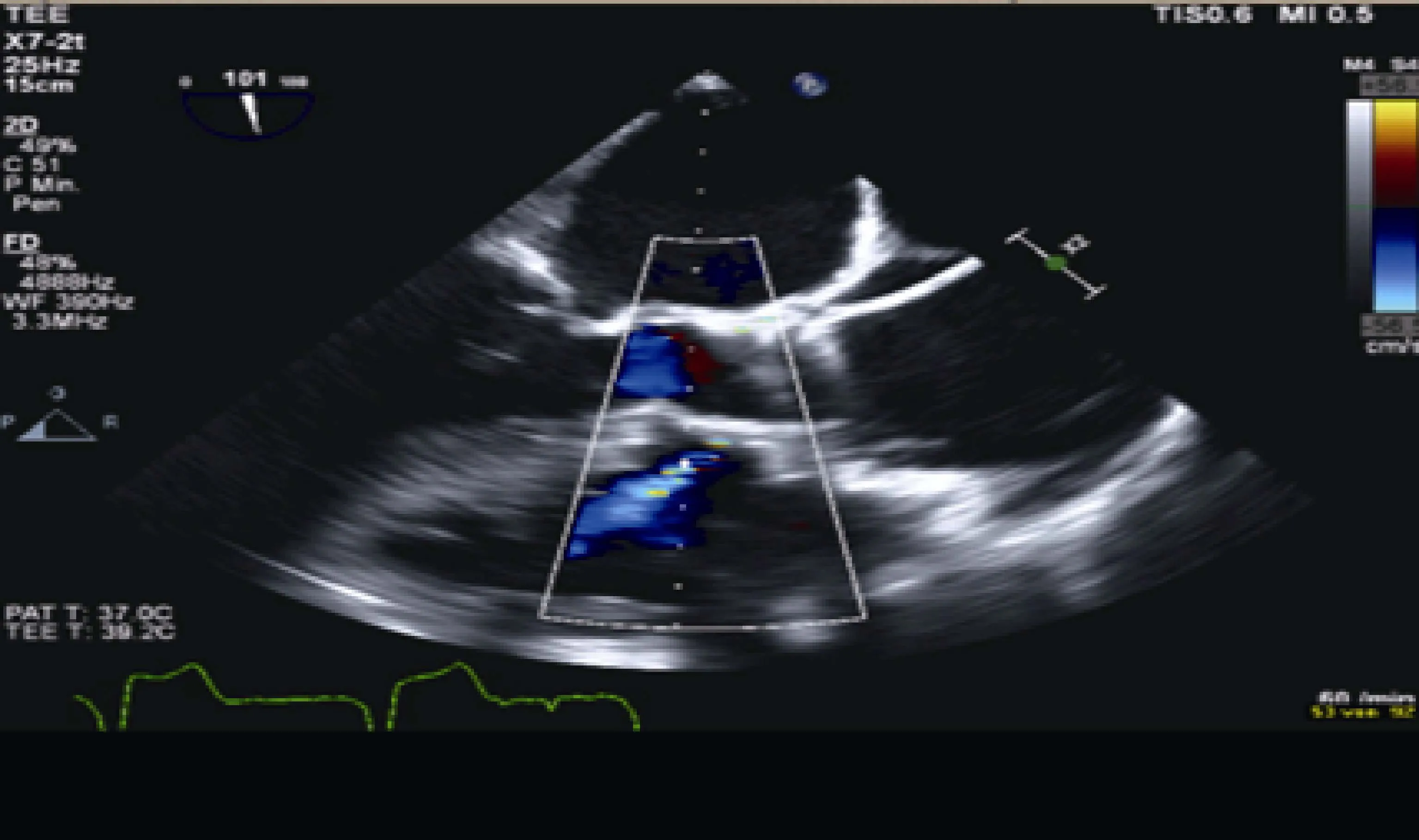
Figure 2. Periprocedural TOE post transcatheter aortic implantation of a 29 mm Edwards Sapien-3 prosthesissmall left to right shunt stemmed from aortic tear/rupture into the right ventricle. Ascending aorta aneurysm with diameter 5.4 cm. TOE: transesophageal echocardiography.
Based on the echocardiographic, angiographic findings combined with the hemodynamically stable course of the patient during hospitalization, a conservative treatment was followed. An arterial blood pressure control was performed due to aortic aneurysm and in an attempt to reduce the shunt’s pressure/volume. Notably, the turbulent flow of the shunt and the simultaneous paravalvular aortic regurgitation rendered our patient as a high risk for endocarditis requiring life-long antibiotic prophylaxis. The patient was improved significantly and discharged after 25 day hospitalization. If there is no improvement of heart failure symptoms despite the combination of optimal medical therapy and TAVR,an implantable cardioverter defibrillator should be considered after three months.
The pre procedural MSCT has been established as the gold standard for transcatheter heart valve sizing (THV;more than 20% over sizing prevention), access-site selection and identification of anatomical factors predisposing to TAVR complication such as severe left ventricular outflow tract (LVOT), intraventricular septum (IVS) or valve calcification, severe asymmetric sub-aortic LV hypertrophy or aortic annulus.[1,2]In our case, three balloon inflations were performed under rapid ventricular pacing. The number of balloon dilatations is a major predisposing factor for aortic rupture.[1,3]The aortic root rupture constitutes a rare, major,non-access site-related vascular complication.[2,4]The aortic rupture could be classified as intrannular, subannular, suprannular or combined, according to its anatomical loca-tions.[3]The most frequently rupture types have been documented in the annulus-area (67.7%) and sinus of valsalva(16.1%) and less often in the LVOT (9.7%) or sinotubular junction (6.4%).[1,2]
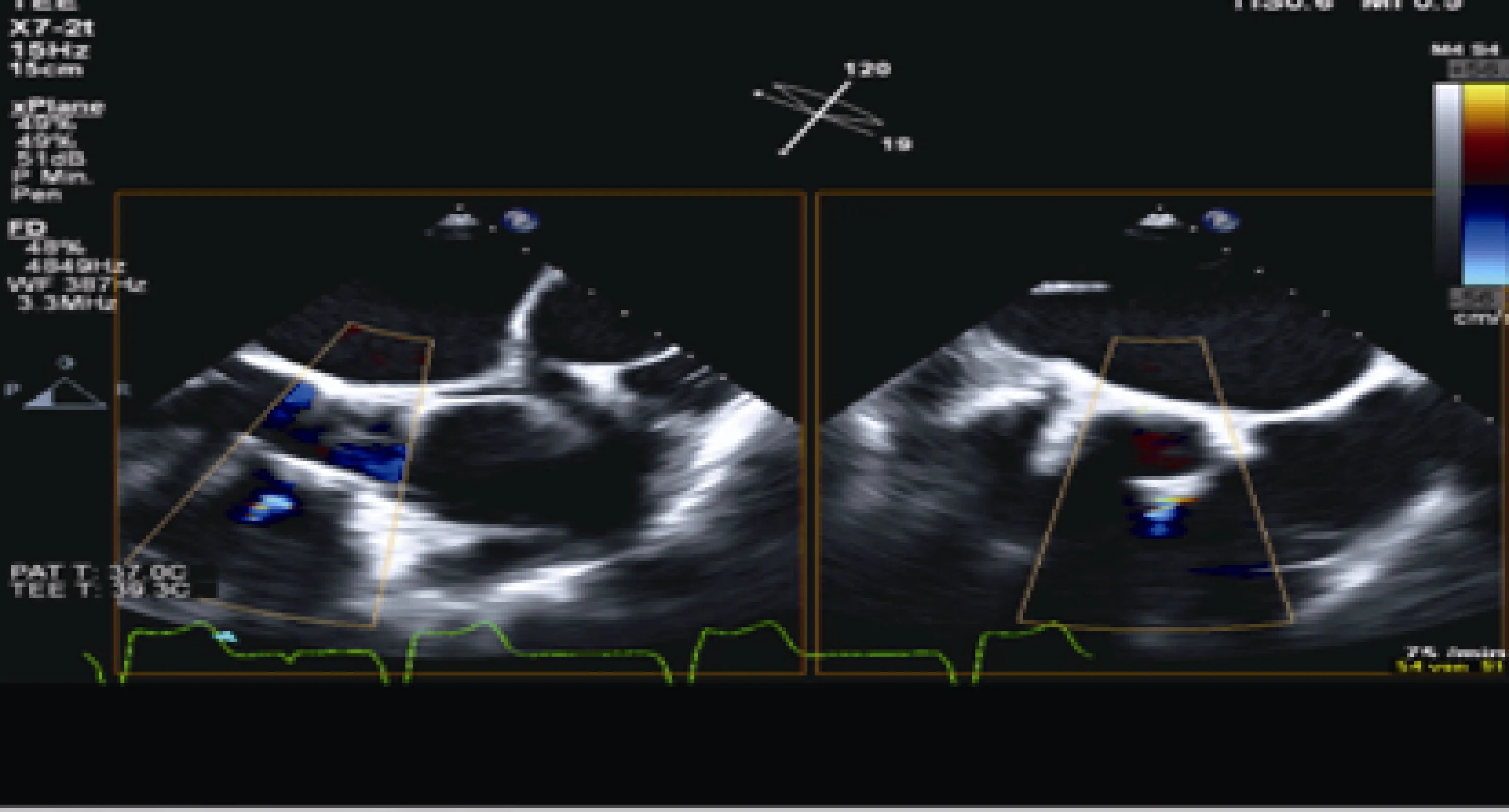
Figure 3. TOE long-axis (LAX) view, 120 degrees and orthogonal plane. Small left to right shunt from a valve tear/rupture into the right ventricle as result of an iatrogenic perimembranous ventricular septal defect. TOE: transesophageal echocardiography.
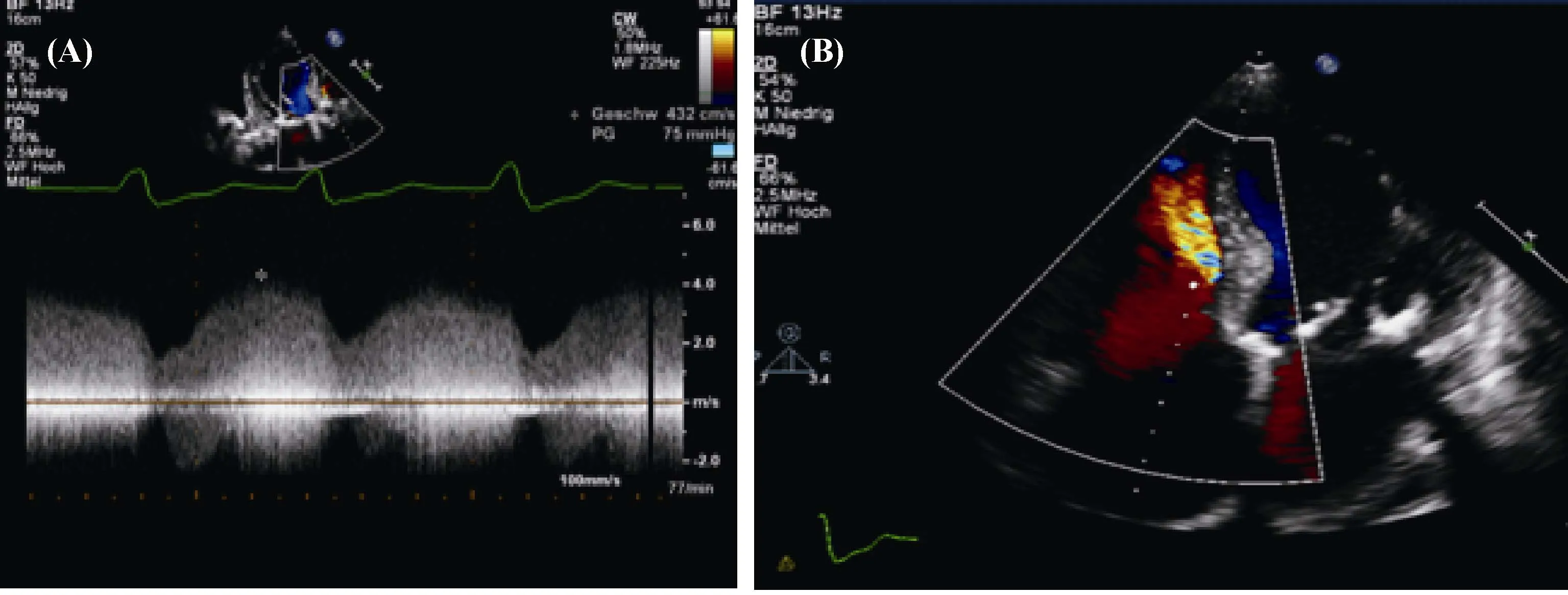
Figure 4. Presence of the VSD-Jet. (A): TTE presence of a continuous flow during systolic- and diastolic period (systolic predominance)through the VSD ending in the right ventricle (left to right direction); (B): the presence of the jet is clearly demonstrated in the apical four chamber view. TTE: transthoracic echocardiogram; VSD: ventricular septal defect.

Figure 5. TTE 5 chamber and 3 chamber apical view: a jet with continuous flow through the VSD (left to right direction). A mild paravalvular leak due to prosthesis malposition to the aortic annulus. TTE: transthoracic echocardiogram; VSD: ventricular septal defect.
The iatrogenic aortic rupture can be asymptomatic or lead to rapid hemodynamic instability (tamponade, bleeding,hematoma, myocardial injury/infarction).[3]The surgical or conservative therapy depends on the localization, the defect size, the patient’s hemodynamic status as well as the Heart Team’s individual decision. Sub-annular of LV free myocardial wall rupture and supra-annular might require an emergency operation.[2–4]Whereas, a small intrannular or intraventricular septum rupture could be treated conservatively.[3,4]Finally, the optimal therapy for asymptomatic aortic rupture post TAVI remains controversial.
The balloon aortic valvuloplasty (BAV) is performed as a bridge to TAVR in high risk patients with severe left ventricular dysfunction or cardiogenic shock.[5–8]A successful BAV might increase the cardiac output and aortic valve area or even decrease transvalvular gradient (up to 30-50%),contributing to haemodynamical improvement.[8–10]The TAVR should be avoided in patients without significant improvement post successful BAV.[7]Post BAV aortic regurgitation could stem from either aortic annulus or leaflet rupture.[11]
The peri- and post-procedural TTE /TOE are crucial for the aortic rupture identification and shunt quantification.TTE/TOE could be challenging in case of intra-annular or sub-annular rupture due to extensive native valve calcifications, the shadowing effect or the prosthetic material reflectance. The non-invasive Qp/Qs evaluation as well as pressure difference between the left and right ventricle contributed to accurate shunt classification as restrictive or no restrictive.[12]
References
1 Barbanti M, Yang TH, Rodès Cabau J, et al. Anatomical and procedural features associated with aortic root rupture during balloon-expandable transcatheter aortic valve replacement.Circulation 2013; 128: 244–253.
2 Barbanti M. Avoiding coronary occlusion and root rupture in TAVI – the role of pre-procedural imaging and prosthesis selection. Interventional Cardiology 2015; 10: 94–97.
3 Pasic M, Unbehaun A, Buz S, et al. Annular rupture during transcatheter aortic valve replacement classification, pathophysiology, diagnostics, treatment approaches, and prevention.JACC Cardiovasc Interv 2015; 8(1 Pt A): 1.
4 Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document. J Thorac Cardiovasc Surg 2013; 145: 6–23.
5 Nwaejike N, Mills K, Stables R, Field M. Balloon aortic valvuloplasty as a bridge to aortic valve surgery for severe aortic stenosis. Interact Cardiovasc Thorac Surg 2015; 20: 429–435.
6 Hara H, Pedersen WR, Ladich E, et al. Percutaneous balloon aortic valvuloplasty revisited time for a renaissance? Circulation 2007; 115: e334–e338.
7 Altarabsheh SE, Greason KL, Schaff HV, et al. Staged balloon aortic valvuloplasty before standard aortic valve replacement in selected patients with severe aortic valve stenosis. Tex Heart Inst J 2014; 41: 152–158.
8 Pedersen WR, Goldenberg IF, Feldman TE, et al. Balloon aortic valvuloplasty in the tavi era: a review of current technique and uses in stand-alone, bridging, and predilation settings. Cardiac Interventions 2010; 77–84.
9 Feldman TE, Sanborn TA, O’Neill WW. Balloon aortic and pulmonic valvuloplasty. Interventional Cardiology 2005;29–48.
10 Pedersen WR, Goldenberg IF, Pedersen CW, et al. Balloon aortic valvuloplasty in high risk aortic stenosis patients with left ventricular ejection fractions < 20%. Catheter Cardiovasc Interv 2014; 84: 824–831.
11 Percutaneous balloon aortic valvuloplasty acute and 30-day follow-up results in 674 patients from the NHLBI balloon valvuloplasty registry. Circulation 1991; 84: 2383–2397.
12 Kitabatake A, Inoue M, Asao M, et al. Noninvasive evaluation of the ratio of pulmonary to systemic flow in atrial septal defect by duplex Doppler echocardiography. Circulation 1984;69: 73–79.
 Journal of Geriatric Cardiology2018年1期
Journal of Geriatric Cardiology2018年1期
- Journal of Geriatric Cardiology的其它文章
- Transcatheter aortic valve replacement and stroke: a comprehensive review
- The role of echocardiography and CT angiography in transcatheter aortic valve implantation patients
- Transcatheter versus surgical aortic valve replacement in severe, symptomatic aortic stenosis
- Antithrombotic therapy in TAVI
- Endocarditis after transcatheter aortic valve implantation: a current assessment
- TAVR in 2017―What we know? What to expect?
