Spontaneous pregnancy after vaginoplasty in a patient presenting a congenital vaginal aplasia
Ferjaoui Mohamed Aimen, Youssef Atef, Gharrad Majed, Achour Radhouane, Mbarki Manel, Malek Monia, Néji Khaled, Reziga Hedi
1Department B of Gynecology and Obstetrics, the Maternity Hospital of Tunis (CMNT), Tunis Medical School, Tunisia
2Department of Gynecological and Obstetrical Emergencies, the Maternity Hospital of Tunis (CMNT), Tunis Medical School, Tunisia
Spontaneous pregnancy after vaginoplasty in a patient presenting a congenital vaginal aplasia
Ferjaoui Mohamed Aimen1*, Youssef Atef1, Gharrad Majed1, Achour Radhouane2, Mbarki Manel1, Malek Monia1, Néji Khaled2, Reziga Hedi1
1Department B of Gynecology and Obstetrics, the Maternity Hospital of Tunis (CMNT), Tunis Medical School, Tunisia
2Department of Gynecological and Obstetrical Emergencies, the Maternity Hospital of Tunis (CMNT), Tunis Medical School, Tunisia
Vaginal aplasia Vaginoplasty Fertility
The vaginal aplasia is a rare Mullerian duct malformation characterized by the absence of the vagina. The management of this malformation is based on surgery to restore a normal sexual life and eventually to hope having a normal fertility. In this case, we presented a spontaneous pregnancy in a 15 year-old girl who underwent a vaginoplasty with re-implantation of the uterus corpus in the neovagina.
1. Introduction
Vaginal aplasia is a congenital affection characterized by the absence of the vagina. It is a rare anomaly, with a reported frequency of 1 in 4 000 to 1 in 10 500 female births. In 10% of cases, vaginal aplasia is associated with a normal development of the uterus and the endometrium [1]. Simple vaginal aplasia is to be differentiated from the Mayer-Rokitansky-Kuster-Hauser which is characterized by an aplasia of the uterus, the cervix and the vagina with or without renal and urinary tract abnormalities.
Patients with a simple vaginal aplasia complain usually from cyclic pelvic pain secondary of menstrual retention. The management of this rare anomaly is based on surgery consisting on creating a neovagina to allow firstly a normal sexual life for patient and secondarily to restore the fertility prognosis. We report a rare case of spontaneous pregnancy in a patient with congenital vaginal aplasia after vaginoplasty and uterine corpus re-implantation in the neovagina.
2. Case report
A 15 year-old girl, without any medical history, complained of primary amenorrhoea and cyclic pelvic pain. Clinical examination showed a normal general development, appropriate general feminization and normally developed vulva. Vagina was absent and replaced by a small blind cup (Figure 1).
Rectal examination showed the presence of uterus. Ultrasound examination confirmed the presence of uterus with a normal endometrium and follicular ovaries; there were no renal or urinary tract abnormalities. A MRI examination confirmed the diagnosis of simple cervico-vaginal aplasia with a normal uterine corpus and endometrium (Figure 2). Biology examination and hormone assays were normal.

?Figure 1. Absence of the vagina, replaced by a blind cup.
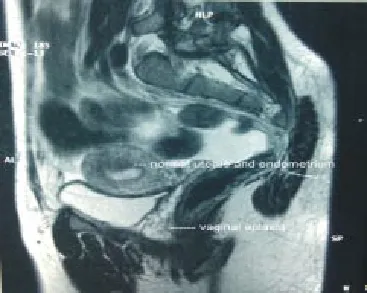
Figure 2. MRI aspect with a sagittal incidence showing the presence of normal and functional uterus and endometrium associated with a cervicovaginal aplasia.
The patient underwent a vaginoplastic procedure after dissection of the recto-vesical space and creating a neovagina with an epidermal graft and a re-implantation of the uterus corpus in the neovagina.
In the immediate post-operative examination the neovagina had a depth of 6 cm (Figure 3). The patient had regular vaginal expansion with Hegar probes during three months. A control examination after 3 months showed a neovagina satisfactory depth of 8 cm.
Twelve months later, the patient presented, in the emergencies department, an acute pelvic pain with vaginal bleeding. Clinical examination, utrasound and HCG assay were in favor of a miscarriage.
Histologic examination of the expelled tissue confirmed the diagnosis. The patient recognizes to have normal sexual intercourse since 5 months however she complained of dyspareunia.

Figure 3. A 10 days post operative aspect (A) showing the depth of the neovagina was 6 cm (B).
3. Discussion
Approximately 7% of girls have an anatomic malformation in their genital tract, diagnosed before or after puberty [2]. To understand the mechanism of the reproductive tract malformation, an embryologic consideration must be reviewed. Reproductive tract development begins at 6–7 weeks gestational age [3]. In the case of female fetus, the Mullerian ducts will begin to fuse around 6–7 weeks of gestational age and this fusion continues through 14 weeks. Once fusion is complete, canalization occurs to form the uterine cavity. At around 12 weeks gestational age, the most caudal portions of the Mullerian ducts begin to fuse with the sinovaginal bulb, forming the vagina, with the top third originating from the Mullerian ducts and the lower third originating from the urogenital sinus. Subsequently, the vaginal canal must go through a process of fusion and absorption with canalization to result in a normal vaginal cavity [3]. Both the lower vagina and hymen therefore originate from the urogenital sinus, whereas the fallopian tube, uterus, cervix, and upper vagina originate from Mullerian structures. Based on this embryologic data, the American Society of Reproductive Medicine (ASRM) established a classification to describe reproductive tract malformation [4]. Concerning cervico-vaginal aplasia, it arises from a defect in development of the Mullerian ducts. The uterine fundus and tubes develop normally but the cervix and vagina fail to develop or canalize [5]. Cervico-vaginal aplasia has been classified as 1b as per the ASRM classification [6].
Vaginal aplasia can associated with a normal and functional uterus, endometrium and Fallopian tubes [6] or be a part of the Mayer-Rokitansky-Kuster-Hauser syndrome presenting as a vaginal atresia and varying degrees of uterine aplasia ranging from rudimentary uterus (or hemi-uteri) to complete uterine agenesis [7].
Clinically, simple vaginal aplasia or cervico-vaginal aplasia (outside the MRKH syndrome) is expressed by cyclic pelvic pain and primary amenorrhoea. Clinical examination showed an ageappropriate female secondary sexual characters and normal appeared external vulva [5]. MRI pelvic examination is the gold standard to
establish a precise idea about intra-abdominal genital organ and is very useful to choose the appropriate surgical technique to manage the reproductive tract malformation [8]. 70% of all patients presenting vaginal aplasia presents endometriosis lesion because of the reflux of menstrual bleeding in the Fallopian tube [5]. Endometriosis lesions are a prognosis factor for fertility after surgical management of vaginal aplasia.
The management of vaginal aplasia or cervico-vaginal aplasia is based on surgery. The surgical approach has many goals: firstly to establish sexual intercourse and normal self-imaging. The secondary goal would be to restore regular menstrual flow and if possible fertility [9].
Surgical management can be a cervical canalization combined with vaginoplasty, a relatively simple procedure with higher risk of restenosis and infection, or vaginoplasty associated to an uterovaginal anastomosis, these procedures are technically more difficult than canalization procedures and aim to anastomose the uterine cavity with the neovagina [10]. With the last surgical technique, the rate of restenosis of the cervical region was much lower and only 22% of patients required a reoperation [10]. Fertility in patients managed for vaginal aplasia is low as compared with the general population. Factors that compromise fertility in these patients are associated upper reproductive tract malformation, pelvic endometriosis and adherences, previous unsuccessful attempts at canalization of the cervix, restenosis of the re-implantation between the uterus corpus and the neovagina, hematosalpinx [10,11]. The lack of or an abnormal endocervical glandular function has been implicated in the case of infertility in these patients [12].
Fujimoto et al. in their review of patients with cervical atresia published in 1997 noted that there were no successful spontaneous pregnancies recorded up until then in patients with cervico-vaginal atresia [5]. Deffarges et al. reported two spontaneous pregnancies in patients with cervico-vaginal atresia [10]. The major goal to operate these patients is to restore a normal sexual life. Unfortunately, there is no study to compare sexuality and the quality of sexual life between different surgical techniques to manage the vaginal aplasia, but it seems that skin grafting vaginoplasty provides a satisfactory sexual intercourse, to check with larger studies. In the case of our patient, she described dyspareunia with a global satisfactory sexual experience.
Vaginal and cervico-vaginal aplasia is a rare congenital malformation characterized by the absence of the vagina in patient with normal development, age-appropriate female secondary sexual characters and normal appeared external vulva. The management of this malformation is based on surgery wit psychological support and sexual advices and care. Commonly, the fertility prognosis is bad but some spontaneous pregnancies are reported. The real challenge is to make an earlier diagnosis of the malformation to ovoid endometriosis lesion and to preserve a potential fertility.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Griffin JE, Edwards C, Madden JD, Harrod MJ, Wilson JD. Congenital absence of the vagina. The Mayer-Rokitansky-Kuster-Hauser syndrome. Ann Intern Med 1976; 85: 224-236.
[2] Breech LL, Laufer MR. Mullerian anomalies. Obstet Gynecol Clin North Am 2009; 36: 47.
[3] Simpson JL. Genetics of the female reproductive ducts. Am J Med Genet 1999; 89: 224.
[4] Buttram VC Jr, Gibbons WE. Mullerian anomalies: a proposed classification. (An analysis of 144 cases). Fertil Steril 1979; 32: 40.
[5] Fujimoto VY, Miller JH, Klein NA, Soules MR. Congenital cervical atresia: Report of seven cases and review of the literature. Am J Obstet Gynecol 1997; 177(6): 1419-1425.
[6] Acién P1, Acién MI, Quereda F, Santoyo T. Cervicovaginal agenesis: spontaneous gestation at term after previous reimplantation of the uterine corpus in a neovagina: case report. Hum Reprod 2008; 23(3): 548-553.
[7] Morcel K, Camborieux L, Guerrier D. Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome. Orphanet J Rare Dis 2007; 14(2): 13.
[8] Acién P, Acién M. The presentation and management of complex female genital malformations. Hum Reprod 2016; 22: 48-69.
[9] Rock JA, Schlaff WD, Zacur HA, Jones HW Jr. The clinical management of congenital absence of the uterine cervix. Int J Gynaecol Obstet 1984; 22(3): 231-235.
[10] Deffarges JV, Haddad B, Musset R, Paniel BJ. Uterovaginal anastomosis in women with uterine cervix atresia: longterm follow-up and reproductive performance. A study of 18 cases. Hum Reprod 2001; 16(8): 1722-1725.
[11] Rock JA, Roberts CP, Jones HW Jr. Congenital anomalies of the uterine cervix: lessons from 30 cases managed clinically by a common protocol. Fertil Steril 2010; 94(5): 1858-1863.
[12] Thijssen RF, Hollanders JM, Willemsen WN, van der Heyden PM, van Dongen PW, Rolland R. Successful pregnancy after ZIFT in a patient with congenital cervical atresia. Obstet Gynecol 1990; 76: 902-904.
ment heading
10.1016/j.apjr.2016.06.005
*Corresponding author: Ferjaoui Mohamed Aimen, Department B of Gynecology and Obstetrics, The Maternity Hospital of Tunis (CMNT), Tunis Medical School, Tunisia.
E-mail: ferjaoui16@yahoo.fr
ARTICLE INFO
Article history: Received Received in revised form Accepted Available online
 Asian Pacific Journal of Reproduction2016年4期
Asian Pacific Journal of Reproduction2016年4期
- Asian Pacific Journal of Reproduction的其它文章
- Evaluation of polymorphonuclear (PMN) cells in cervical sample as a diagnostic technique for detection of subclinical endometritis in dairy cattle
- In vitro polyembryony induction on a critically endangered fern, Pteris tripartita Sw.
- Natural honey as a cryoprotectant to improve Arab stallion post-thawing sperm parameters
- Effects of pomegranate juice in Tris-based extender on cattle semen quality after chilling and cryopreservation
- The relationship between trace mineral concentrations of amniotic fluid with placenta traits in the pregnancy toxemia Ghezel ewes
- Evaluation of the academic achievement of rural versus urban undergraduate medical students in pharmacology examinations
