lntrahepatic Glissonian approach and outflow vascular occlusion during partial hepatectomy
Feng Xia, Guo Li, Wan-Yee Lau, Kuan-Sheng Ma and Ping Bie
Chongqing, China
lntrahepatic Glissonian approach and outflow vascular occlusion during partial hepatectomy
Feng Xia, Guo Li, Wan-Yee Lau, Kuan-Sheng Ma and Ping Bie
Chongqing, China
Under ultrasound guidance, a blunt suture needle was inserted around the Glissonian pedicle and then sutured. This technique significantly reduced the blood loss and facilitated the procedure of partial hepatectomy. We applied this technique in 182 patients who needed partial hepatectomy. We concluded that this method is simple and easy to occlude the vascular inflow and outflow, and allows an accurate delineation of the anatomic zone and therefore, simplifies the procedure of partial hepatectomy.
hepatectomy;
the Glissonian approach;
blunt needle;
surgical technique
Introduction
Intraoperative bleeding is a major cause of perioperative morbidity and mortality in partial hepatectomy.[1, 2]Various vascular occlusion and hepatic parenchymal transection techniques are currently used to decrease blood loss during liver resection. In many centers, Pringle's maneuver with total vascular inflow occlusion is a common method. However, ischemia-reperfusion injury induced by vascular inflow occlusion to the liver remnant is a major concern, particularly in patients with cirrhosis.[3]Lortat-Jacob et al[4]in 1952 reported the first successful right hepatectomy by ligating the vascular inflow and outflow to the right liver before parenchymal transection. Then, the Glissonian pedicle approach was introduced by Takasaki et al.[5]This approach is to ligate the hepatic hilus and block the vascular inflow to the hepatic section to be resected. Later on, the same group improved the Glissonian pedicle approach in 1990 by transecting the portal triad supplying the hepatic section to be resected within the Glissonian sheath.[6]However, the Glissonian approach is tedious and time-consuming, and causes excessive intraoperative bleeding and even bile leakage after surgery because of the transection of a substantial amount of liver tissue being access to the pedicle.[7]
We used an intraoperative ultrasound to guide a blunt suture needle to ligate the Glissonian pedicle. This technique simplifies the procedure of partial hepatectomy.
Surgical technique
The surgery started with a right subcostal or midline incision with a right horizontal extension as previously described.[8, 9]The liver was fully mobilized after transection of its ligaments attaching the liver to the abdominal wall. Intraoperative ultrasonography (IUS) was performed routinely to delineate the extent of the tumor, to detect the satellite tumors which were not shown on preoperative images, to detect invasion of the tumor into major blood vessels, and to plan and delineate the plane of parenchymal transection. Hepatic hilar dissection was not necessary for hilar occlusion, but cholecystectomy should be routinely performed for right hepatectomy. Low central venous pressure (1-5 cmH2O or 0.74-3.70 mmHg) was needed. Parenchymal transection was carried out using either a clampcrushing technique with a Kelly clamp or with Cavitron Ultrasonic Surgical Aspirator (CUSA, Tyco Healthcare, Mansfield, MA, USA).
To occlude hepatic vascular inflow and outflow, a blunt suture needle (No. 1, 65 mm, 3/8c, BP-5, ETHICON ? Coated VICRYL?, Johnson & Johnson Inc) was used (Fig. 1). IUS was used to position the Glissonian inflow vascular pedicle and the outflowhepatic vein supplying the hepatic section to be resected. The proper site for insertion of the blunt needle was also located under the guidance of IUS. A blunt suture needle was put around the Glissonian pedicle of the left liver, the anterior or the posterior section of the right liver, or the right liver, and around the corresponding hepatic vein (right/middle/left). The two ends of the suture were brought through a short rubber tube (Fig. 1), and they were tightened by pushing the rubber tube against the liver parenchyma to crush the fragile overlying liver tissue. The blunt needle was easy to pass from one side of the Glissonian pedicle and come out from the other side when it just went through liver parenchyma. When the needle encroached into the Glissonian sheath, it should be slightly withdrawn and changed the direction until the needle passed around the Glissonian pedicle smoothly and easily. Putting the needle around the hepatic vein requires a slightly different technique. The fossa between the right and the middle hepatic veins should be dissected first to give a more accurate point of entry/exit of the needle. IUS guidance during the passage of the needle into liver parenchymal around the hepatic vein was useful (Figs. 2, 3). When the needlepenetrates into a hepatic vein, little bleeding can be stopped easily by pressing with the fingers for a few minutes.

Fig. 1.The No. 1 ETHICON? Coated VICRYL? needle-suture and a rubber tube.
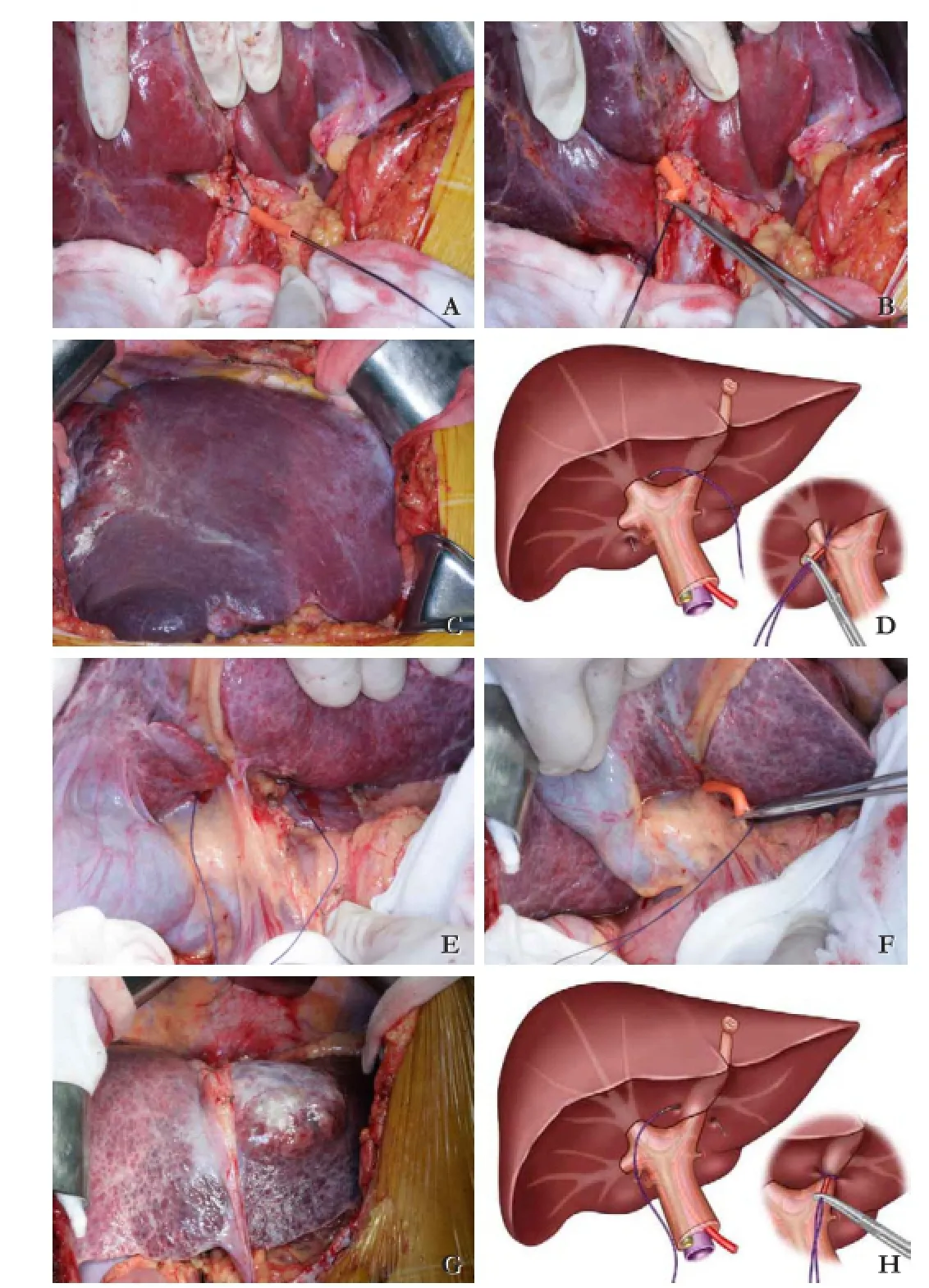
Fig. 2.Ligating the pedicle of right and left half of the liver without hilar dissection.A: sewing with long blunt point needle-suture;B: a rubber tube employed to frap the pedicle by clamp crushing;C: demarcation displayed;D: schematic illustration of the procedure;E,F,G, andH: ligating the pedicle of the left half of the liver similarly.
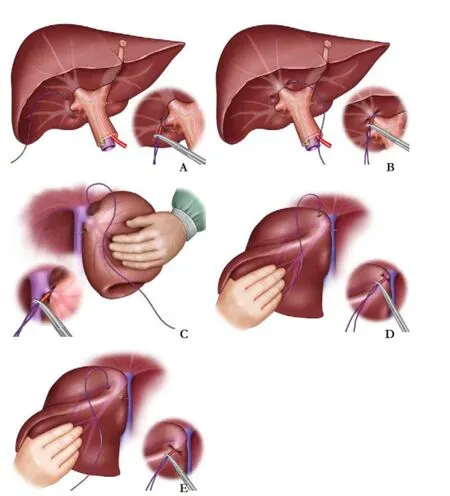
Fig. 3.Schematic illustration of our technique to occlude the inflow and outflow of the liver by sewing the Glissonian sheath of the branch pedicle or hepatic vein with blunt point needle-suture.A: right posterior pedicle;B: right anterior pedicle;C: right hepatic vein;D: middle and left hepatic vein;E: left hepatic vein.
From January 2009 to April 2012, 182 major (n=91) and minor (n=91) liver resections were carried out using this technique. Major hepatectomy was defined as greater than or equal to three Couinaud segments. This procedure can be finished in about 1-3 minutes with very little bleeding. There was no procedure-related mortality or morbidity.
Discussion
The Glissonian pedicle approach has been reported to be safe and reliable for anatomic partial hepatectomy for more than 20 years.[10]The advantage of this method is efficacious in decreasing intraoperative hemorrhage. However, the technique is tedious and time-consuming, with a high incidence of bile leakage after surgery.[7, 10]Sometimes, the bifurcation of the hepatic pedicle is difficult to dissect. Chen et al[7]described a similar technique for anatomical left hepatectomy. In his method, a long curved Kelly clamp is inserted into the hepatic parenchyma on the surface of the hilar transverse fissure above the Glissonian sheath supplying the left liver. The clamp then penetrates the parenchyma at the left inferior margin of the hilar transverse fissure. The jaws of the clamp are then slightly opened, and the tip of a No. 8 suture is grasped and is pulled out through the clamp's tunnel. The left hepatic pedicle is then ligated. Machado et al[11]described a similar technique using intrahepatic Glissonian access with a large curved Mixter clamp for segmental liver resection in cirrhotic patients. However, this technique may cause more bleeding from the tunnel through which the Kelly clamp or Mixter clamp passes, especially in cirrhotic patients with portal vein hypertension.
Chang et al[12]stated another similar technique with a specially designed needle called the Chang's needle (a straight inner needle with a hook near its top to catch the thread and an 18-gauge stainless steel external sheath). The needle is inserted on the surface through the whole depth of the liver parenchyma where it catches one end of a No. 1 thread from below, and the end of this thread is pulled out of the liver surface. The maneuver is repeated once again 3-5 cm away from the previous insertion. Then, the two ends of the thread are brought together, tightened and a secure knot is made to occlude the vascular flow within this part of the liver. Chang's maneuver can be used to occlude the inflow and outflow vascular pathway for small hepatic resections. However, it is not suitable for hilar Glissonian pedicles because the needle is straight.
Our method using a long blunt suture needle is technically easier and causes less bleeding. This technique was firstly used in a patient with a critical condition. A big tumor located in the left liver ruptured during separation of its adhesions to the abdominal wall. There was severe bleeding which was difficult to control with the routine methods of stitching or packing. The bleeding stopped immediately when the left Glissonian pedicle was blocked with this procedure. Our technique does not require a special instrument as reported by Chang et al.[12]To use a rubber tube to break the liver tissue and to compress the vessel are less likely to cause direct injury to the vasculature. When the bifurcation of the vessel is very deep within the liver parenchyma, ultrasound guidance is very useful to delineate its position. This new technique demarcates the ischemic zone to be resected easily. Since this technique requires no special instrument, it can be learned easily and vascular occlusion can be completed within 1 minute.
In conclusion, this technique is simple and useful in occluding the vascular inflow and outflow, and allows accurate delineation of the anatomic zone of the liver to be resected during partial hepatectomy.
Contributors:XF proposed the study. XF and LG wrote the fi rst draft. LWY contributed to the revision of draft. All authors contributed to the design and interpretation of the study and to further drafts. XF is the guarantor.
Funding:This work was supported by a grant from Scienti fi c and Technological Project of Chongqing city (CSTC2012gg-yyjs10016).Ethical approval:Not needed.
Competing interest:No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, et al. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg 2004;240:698-710.
2 Kuvshinoff B, Fong Y. Surgical therapy of liver metastases. Semin Oncol 2007;34:177-185.
3 Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg 2000;191:38-46.
4 Lortat-Jacob JL, Robert HG. Well defined technic for right hepatectomy. Presse Med 1952;60:549-551.
5 Takasaki K, Kobayashi S, Tanaka S, Muto H, Watayo T, Saito A, et al. Newly developed systematized hepatectomy by Glissonean pedicle transection method. Shujutsu 1986;40:7-14.
6 Launois B. The intrahepatic glissonian approach to liver resection. In: Blumgart LH, Fong Y (eds). Surgery of the liver and biliary tract. London: WB Saunders; 2000:1698-1703.
7 Chen XP, Qiu FZ. A simple technique ligating the corresponding inflow and outflow vessels during anatomical left hepatectomy. Langenbecks Arch Surg 2008;393:227-234.
8 Xia F, Lau WY, Qian C, Ma K, Li X, Bie P. Continuous occlusion of hepatic artery proper for prevention of blood loss in partial hepatectomy for ruptured hepatocellular carcinoma: a case-matched comparative study. Ann Surg Oncol 2011;18:1638-1643.
9 Xia F, Lau WY, Qian C, Wang S, Ma K, Bie P. Surgical treatment of giant liver hemangiomas: enucleation with continuous occlusion of hepatic artery proper and intermittent Pringle maneuver. World J Surg 2010;34:2162- 2167.
10 Yamamoto M, Katagiri S, Ariizumi S, Kotera Y, Takahashi Y. Glissonean pedicle transecton method for liver surgery (with video). J Hepatobiliary Pancreat Sci 2012;19:3-8.
11 Machado MA, Herman P, Machado MC. Intrahepatic Glissonian approach for pedicle control during anatomic mesohepatectomy. Surgery 2007;141:533-537.
12 Chang YC, Nagasue N. Blocking intrahepatic inflow and backflow using Chang's needle during hepatic resection: Chang's maneuver. HPB (Oxford) 2008;10:244-248.
Received November 1, 2012
Accepted after revision September 4, 2013
(Hepatobiliary Pancreat Dis Int 2014;13:101-104)
Author Affiliations: Institute of Hepatobiliary Surgery, Southwest Hospital, Southwest Cancer Center, Third Military Medical University, Chongqing, China (Xia F, Li G, Lau WY, Ma KS and Bie P); Faculty of Medicine, the Chinese University of Hong Kong, Hong Kong, China (Lau WY)
Feng Xia, MD, PhD, Institute of Hepatobiliary Surgery, Southwest Hospital, Southwest Cancer Center, Third Military Medical University, Chongqing, China (Tel: 86-23-68765797; Fax: 86-23- 65317637; Email: frankfxia@163.com)
? 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60015-1
 Hepatobiliary & Pancreatic Diseases International2014年1期
Hepatobiliary & Pancreatic Diseases International2014年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Samaritan donor interchange in living donor liver transplantation
- Complex hepatic outflow reconstruction in domino liver transplantation
- Novel en-bloc resection of locally advanced hilar cholangiocarcinoma: the Rex recess approach
- KAI1 inhibits lymphangiogenesis and lymphatic metastasis of pancreatic cancer in vivo
- Effect of CD74 on the prognosis of patients with resectable pancreatic cancer
- Blood group type antigens in pancreatic intraductal papillary mucinous neoplasms
