Evaluation of anti-parkinson’s activity of gentisic acid in different animal models
Kabra MP, Bhandari SS, Sharma A, Gupta RB
Department of Pharmacology, Kota College of Pharmacy, Kota (Raj.), India
Evaluation of anti-parkinson’s activity of gentisic acid in different animal models
Kabra MP*, Bhandari SS, Sharma A, Gupta RB
Department of Pharmacology, Kota College of Pharmacy, Kota (Raj.), India
Objective: To evaluate the neuroprotective activity of Gentisic acid in PD. The study was conducted on swiss albinFo mice (20-25 g) & wistar rats (200-250 g). Methods: Three behavioural models namely, Haloperidol induced catalepsy, Reserpine antagonism and Haloperidol induce orofacial dyskinesia were employed in this study, Swiss Albino mice (20-25 g) were used in first two models while Wistar rats (200-250 g) used in last one model. There are five group (n=6) in each animal model. Various behavior activity/parameter (cataleptic behavior, horizontal movements, rearing & grooming frequencies and Dyskinesia activity like vacuous chewing & tongue protrusion) in different animal models were used to evaluate the anti-Parkinson’s activity of Gentisic acid. Results: Gentisic acid showed a significant (P<0.01) reduction in the duration of cataleptic behavior dose dependently when compared to haloperidol control group. Gentisic acid shows dose dependant increase in the frequency of horizontal movement and rearing behavior when compared to the Reserpine control group. But, the effect of Gentisic acid on the frequency of grooming behavior was found to be insignificant. Gentisic acid (80 mg/kg) showed a significant (P<0.05) decrease in the frequency of vacuous chewing & tongue protrusion but the other dose tested were found to be insignificant in this respect. Conclusions: Results shows that the Gentisic acid produced dose dependent neuroprotective activity in different animal models of PD.
ARTICLE INFO
Article history:
Received 8 August 2013
Received in revised form 15 September 2013
Accepted 24 September 2013
Available online 20 June 2014
Gentisic acid
1. Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disorder worldwide and is characterized by the progressive loss of dopaminergic neurons in substantia nigra (SN)[1]. The clinical symptoms of PD mainly include rest tremors, rigidity, bradykinesia and postural abnormalities[2]. A growing body of evidence support the role in PD, of an impaired function of the mitochondria[3]. The exact cause of Parkinson’s disease still is not known, but there is a growing body of evidence that nigral neurons may be damaged by cytotoxic substances known as free radicals. Free radicals are thought to be produced locally within the basal ganglia and to lead to progressive damage to and death of substantia nigra neurons[4].
Gentisic acid (dihydroxybenzoic acid) is an active metabolite of salicylic acid. Reported activity of Gentisic acid are antioxidant[5], antiatherogenic[6], anticancer[7], skeletal muscle relaxant[8]. Gentisic acid inhibits LDL oxidation in a concentration-dependent manner. It significantly inhibit the formation of cholesterol ester hydro peroxides in plasma, and was consumed after the depletion of ascorbic acid and reduced form of coenzyme Q-10 (CoQH2-10), whereas concentrations of other antioxidants remained unchanged. Gentisic acid had a potent free radical scavenging activity with a minimal chelating effect[9]. The present study is carried out to evaluate the anti-Parkinson’s activity of Gentisic acid in different animal models due to anit-oxidant activity.
2. Materials and methods
2.1. Experimental animals
The study was conducted on Albino mice (20-25 g) & wistar rats (200-250 g) and maintained under standardconditions (room temperature 24-27 ℃ and humidity 60-65%) with 12 h light and dark cycle. The food in the form of dry pellets (Amrut Lab., Pune) and water were available ad libitum. The animal experiments were approved by the IAEC.
2.2. Chemicals and drugs
Gentisic acid (Sigma Aldrich Pvt. Ltd, USA), Glacial acetic acid (Research Lab Fine chemical Industries, Mumbai, India), Haloperidol (marketed as SERENACE INJ.), L-dopa (SYNDOPA? 110, Sun Pharmaceuticals Ind. Ltd., Silvasa, India), Reserpine (Sigma Aldrich Pvt. Ltd., USA)
2.3. Experiment design
2.3.1. Acute toxicity studies
The acute toxicity study was taken from Material Safety Data Sheet provided by Sigma Aldrich. It is 800 mg/kg, p.o. for rat & 4 500 mg/kg, p.o. for mice.
2.3.2. Haloperidol induced catalepsy in mice[10]
Albino mice of either sex weighing 20-25 g was divided into five groups of six animals each (n=6). The animals were allowed to adapt to the box for 2 min. A cataleptic behavior was measured with a “High bar test method”. The standard (L-dopa) drug was administered by intraperitoneal route and test drug was administered by oral route, half an hour prior to the Haloperidol administration. Catalepsy score was measured for each hour upto 4 h after Haloperidol administration, by gently placing both the forepaws of the mouse over a metal bar (diameter 2-5 mm) suspended 6 cm above the table top. The intensity of catalepsy was assessed by counting time in seconds until the mouse brought both forepaws down to the table top, with a maximum cut-off time of 180 s.
2.3.3. Reserpine antagonism in mice[10]
Mice were administered with Reserpine (5 mg/kg, i.p.). After 24 h, test drug or standard drugs were administered 30 min prior to observation. Mice were placed on floor of Perspex container having dimension 30×26×20 cm. Behavioral assessment was recorded for 10 min. In this the horizontal movements, rearing & grooming frequencies were measured.
2.3.4. Haloperidol induce orofacial dyskinesia in rat[11]
Dyskinesia is characterized by vacuous chewing & tongue protrusion. Five groups of wistar rats (n=6) were used. Haloperidol was administered in the rats for a period of 21 d to induce oral dyskinesia. Test agent was administered once daily in the morning for a period of 21 d and behavioural assessments was performed at 7th, 14th, 21th day.
2.3.5. Statistical analysis
The Statistical analysis was performed by using One Way ANOVA followed by Dunnet’s comparison test and studentt-test (unpaired).The values are expressed as mean ± SEM and the P<0.05 was taken as significant.
3. Results
3.1. Haloperidol induced catalepsy in mice
Treatment with L-dopa (10 mg/kg, i.p) showed a significant (P<0.01) reduction in the cataleptic behavior between 60 to 180 min of time interval as compared to the haloperidol treated group. Treatment with Gentisic acid showed a significant (P<0.01) reduction in the duration of cataleptic behavior dose dependently when compared to haloperidol treated group.
3.2. Effect of gentisic acid on reserpine antagonism in mice
L-dopa (10 mg/kg, i.p) showed a significant (P<0.01) increase in the frequency of horizontal movement, rearing behavior and grooming behavior. Both dose of Gentisic acid (225 mg/kg and 450 mg/kg i.p.) showed significant (P<0.05) (P<0.01) respectively increase in the frequency of horizontal movement and rearing behavior when compared to the Reserpine treated group, but the effect of both dose of Gentisic acid on the frequency of grooming behavior was found to be insignificant.
3.3. Effects of gentisic acid on haloperidol induce orofacial dyskinesia in wistar rat
L-dopa (10 mg/kg, i.p.) showed a significant (P<0.05) recovery of orofacial dyskinesia as evidenced by decrease in the frequency of vacuous chewing movement and tongueprotrusion. However, Gentisic acid (80 mg/kg) showed a significant (P<0.05) decrease in the frequency of vacuous chewing & tongue protrusion while Gentisic acid (40 mg/kg) was found to be insignificant in this respect.

Table 1 Effect of gentisic acid in haloperidol induced catalepsy in mice.
4. Discussion
Animal models of Parkinson’s disease are widely used to investigate its pathophysiological mechanisms and for exploring potential treatments[12,13]. Typically, models of PD are characterized by measures of akinesia, such as in bar test for immobility.
Neuroleptics such as haloperidol can produce a sustained but reversible akinesia, due to blockade of dopamine D2receptors and this neuroleptic-induced Parkinsonism is a major side effect of their use in treatment of schizophrenia. D2antagonists may act directly to reduce the ability of cortical and basal ganglia motor pathways to generate descending commands. Neuroleptics have thus been used as an acute model of Parkinson[14]. The central dopaminergic function and evaluation of dopamine agonistic activity was carried out by observing the cataleptic behavior in mice. Haloperidol blocks the dopamine D2receptors in the brain and precipitates the extra pyramidal side effects that can be measured by “Bar test for catalepsy in mice”.
Oral movement is an important symptom presented by a series of neuropsychiatric conditions including Parkinson’s disease[15,16]. In addition, a spontaneous aging-induced oral dyskinesia has been extensively described. Thus, oral dyskinesia may represent the behavioral manifestation resulting from underlying mechanisms shared by different neuropsychiatric conditions. Tardive Dyskinesia is a motor side effect of long term treatment with typical neuroleptics (such as haloperidol) that involves involuntary movements of the face, mouth and tongue, but other different parts of the body may also be affected[17]. Treatment with L-dopa (10 mg/kg, i.p.) significantly attenuated the dyskinetic behavior in rats. Gentisic acid showed a significant attenuation in the frequency of tongue protrusions & VCM at higher doses tested.
In the present investigation, the Reserpine treatment also showed effect on the stereotypic behavior in the mice which was characterized by decrease in frequency of horizontal movements, rearing and grooming behavior. The treatment with L-dopa showed a significant alteration in the stereotypic behavior when compared to Reserpine control group. However, the treatment with Gentisic acid shows dose dependant increase in the frequency of horizontal movement and rearing behavior when compared to the Reserpine control group. But, the effect of Gentisic acid on the frequency of grooming behavior was found to be ineffective. It is also well known that Haloperidol blocks dopamine receptors and may contribute to haloperidol neurotoxicity due to the generation of free radicals and the increase in lipoperoxidation products[18]. This leads to the concomitant increase in the turnover of this amine which therefore remains available for metabolism either by auto oxidation or by oxidative deamination catalyzed by Monoamine oxidase (MAO). Consequently, it may lead to an increase in Dopamine (DA) metabolites along with a reduction in dopamine receptor activation. During this process, hydrogen peroxideis thus formed and becomes an important source of oxidative stress in catecholaminergic neuronal systems[19]. some study states that Haloperidol neurotoxicity to the inhibition of mitochondrial electron transfer with an enhancement of O2and H2O2production[20]. Reactive Oxygen Species (ROS) originating from the oxidation of Dopamine (DA) further participates in the pathogenesis of PD[21]. Oxidative stress generated as a result of mitochondrial dysfunction, particularly mitochondrial complex-1 impairement plays an important role in the PD pathogenesis[21]. Probably, there is not a single factor responsible for neurodegeneration; it appears that several factors are acting in concert.

Table 2 Effect of gentisic acid on frequency of horizontal movement, rearing behavior and grooming behavior.

Table 3 Effect of gentisic acid on haloperidol induce orofacial dyskinesia in wistar rat.
Oxidative stress and consequent cell death could occur in the SNpc under circumstances in which there is (a) an increased dopamine turnover, resulting in excess peroxide formation; (b) a deficiency in glutathione (GSH) content, thereby diminishing the brains capacity to clear H2O2or (c) an increase in reactive iron species, which can promote hydroxyl radical formation[22]. After Gentisic acid treatment, the significant alterations produced in Parkinson’s affected rodents with respect to lipid peroxidation and antioxidant concentration hence signifies its antioxidant potential. This antiperoxide action observed in Gentisic acid treated animals might be due to the suppression of the production of reactive oxygen species. This compound may be found to scavenge free radicals, including hydroxyl anions and reduce the level of lipid peroxidation in Parkinsonian animals. Inhibition of oxidative stress may be one of the possible mechanisms for the anti-Parkinson effects of Gentisic acid.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgement
[1] Lev N, Melamed E, Offen D. Apoptosis and Parkinson’s disease. Prog Neuropsychopharmacol Biol Psychiatry 2003; 27: 245-250.
[2] Singha S, Dikshit M. Apoptotic neuronal death in Parkinson’s disease: involvement of nitric oxide. Brain Res Rev 2007; 54: 233-250.
[3] Emerit J, Edeas M, Bricaire F. Neurodegenerative diseases and oxidative stress. Biomed Pharmacother 2004; 59: 39-46.
[4] Ciccone CD. Free-radical toxicity and antioxidant medications in Parkinson’s disease. Phys Ther 1998; 78: 313-319.
[5] Dinis TC, Madeira VC, Almeida LM. Action of phenolic derivates (acetoaminopehn, salycilate and 5-aminosalycilate) as inhibitors
The authors are thankful to the authorities of Kota College of pharmacy, Kota (Rajasthan) for providing support to the study and other necessary facility like internet surfing, library and other technical support to write a research article. of membrane lipid peroxidation and as peroxyl radical scavengers. Arch Biochem Biophys 1994; 315: 161-169.
[6] Keiko AB, Mitsunobu KT, Daigo M, Hisako T, Shigeru M, Tamio, T, et al, Gentisic acid, an aspirin metabolite, inhibits oxidation of low-density lipoprotein and the formation of cholesterol ester hydro peroxides in human plasma. Eur J Pharmacol 2005; 513: 173-179.
[7] Sharma S, Khan N, Sultana S. Modulatory effect of gentisic acid on the augmentation of biochemical events of tumor promotion stage by benzoyl peroxide and ultraviolet radiation in Swiss albino mice. Toxicol Lett 2004; 153: 293-302.
[8] Cunha JF, Campestrini FD, Scremin A, Calixto JB, Paulino N. The mechanism of gentisic acid-induced relaxation of the guinea pig isolated trachea: the role of potassium channels and vasoactive intestinal peptide receptors. Braz J Med Biol Res 2001; 34: 381-388.
[9] Markus E, Marcela H, Roland H, Stylianos K, Wolfgang S, Irmtraud H, et al. The salicylate metabolite gentisic acid, but not the parent drug, inhibits glucose autoxidation-mediated atherogenic modi¢cation of low density lipoprotein. FEBS Letters 2000; 470: 47-50.
[10] Vogel HG, Vogel WH, Scholkens BA, Sandow J, Muller G. Drug Discovery and Evaluation, Pharmacological Assays. 2nd ed. Heidelburg: Springer; 2002, p. 580-581.
[11] Bishnoi M, Chopra K, Kulkarni SK. Protective effect of Curcumin, the active principle of turmeric (Curcuma longa) in haloperidolinduced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes in rat brain. Pharmacol Biochem Behav 2008; 88: 511-522.
[12] Dawson TM. New animal models for Parkinson’s disease. Cell 2000; 101: 115-118.
[13] Rodriquez DM, Abdala P, Barroso-Chinea P, Obeso J, Gonzdez-Hernandez T. Motor behavioral changes after intracerebroventricular injection of 6-hydroxy dopamine in the rat: an animal model of Parkinson’s disease. Behav Brain Res 2001; 122: 79-92.
[14] Chandra S, Chen X, Rizo J, Jahn R, Sudho TC. A broken α helix in folded α-synuclein. J Biol Chem 2003; 278: 15313-15318.
[15] Jicha GA, Salmone JD. Vacuous jaw movements and feeding deficits in rats with ventrolateral striatal dopamine depletion: possible relations to parkinsonian symptoms. J Neurosci 1991; 11: 3822-3829.
[16] Paille V, Brachet P, Damier P. Role of nigral lesion in the genesis of dyskinesias in a rat model of Parkinson’s disease. Neuroreport 2004; 15: 561-564.
[17] Marin C, Saldana M, Roca-Ferrer J, Bonastre M, Aguilar E, Mullol J. Striatal and nigral COX-2 expression after chronic typical and atypical neuroleptic administration in rats. Prog Neuro-Psychopharmacol Biol Psychiat 2007; 31: 678-682.
[18] Burger ME, Fachineto R, Alves A, Callegari L, Batista TR. Acute reserpine and subchronic haloperidol treatments change synaptosomal brain glutamate uptake and elicit orofacial dyskinesia in rats. Brain Res 2005; 1031: 202-210.
[19] Lohr JB. Oxygen free radicals and neuropsychiatric illness. Arch Gen Psychiat 1991; 48: 1097-1106.
[20] Arniaz SL, Coronel MF, Boveris A. Nitric oxide, superoxide, and hydrogen peroxide production in brain mitochondria after haloperidol treatment. Nitric Oxide 1999; 3: 235-243.
[21] Nehru B, Verma R, Khanna P, Sharma SK. Behavioral alterations in rotenone model of Parkinson’s disease: Attenuation by cotreatment of centrophenoxine. Brain Res 2008; 1201: 122-127.
[22] Jenner P. Oxidative mechanisms in nigral cell death in Parkinson’s disease. Mov Disord 1998; 13: 24-34.
ment heading
10.1016/S2221-6189(14)60031-7
*Corresponding author: Mahaveer Prasad Kabra, Asst. Professor, Department of Pharmacology, Kota College of pharmacy, Kota (Raj.), India.
Tel: 09462528624
E-mail: sanskarkabra@gmail.com
Catalepsy
Parkinson’s disease
Dyskinesia
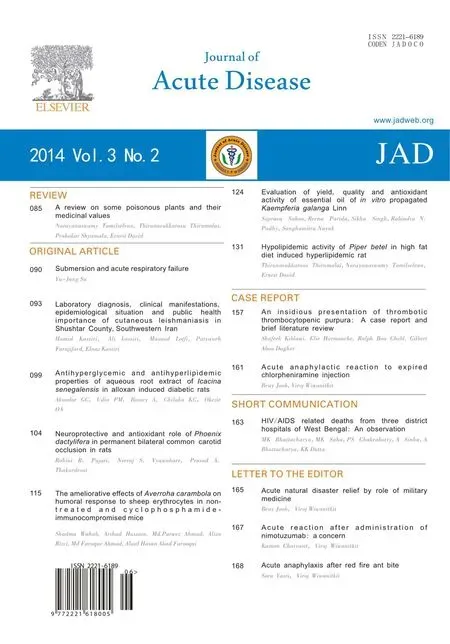 Journal of Acute Disease2014年2期
Journal of Acute Disease2014年2期
- Journal of Acute Disease的其它文章
- Acute anaphylactic reaction to expired chlorpheniramine injection
- An insidious presentation of thrombotic thrombocytopenic purpura: A case report and brief literature review
- Acute anaphylaxis after red fire ant bite
- Acute reaction after administration of nimotuzumab: a concern
- Acute natural disaster relief by role of military medicine
- HIV/AIDS related deaths from three district hospitals of West Bengal: An observation
