Drainage by urostomy bag after blockage of abdominal drain in patients with cirrhosis undergoing hepatectomy
Nanjing, China
Drainage by urostomy bag after blockage of abdominal drain in patients with cirrhosis undergoing hepatectomy
Guo-Qiang Li, Feng Zhang, Hao Lu, Ling Lu, Xiang-Cheng Li, Xue-Hao Wang and Bei-Cheng Sun
Nanjing, China
Abdominal drainage was previously recommended as a post-hepatectomy procedure for patients with cirrhosis. This report introduces a simple technique that prevents leakage of ascitic fl uid after cirrhotic hepatectomy complicated by blockage of the abdominal drain. In 59 patients who had had cirrhotic hepatectomy complicated by leakage of ascites in the drain site after drainage removal between January 2001 and April 2011, 31 underwent suture ligation (sutured group) and 28 were given urostomy bag at the abdominal drainage site (drainage group). The mean length of postoperative hospital stay in the drainage group was shorter than in the sutured group (16.11±2.61 vs 34.23±4.86 days,P=0.000). Meanwhile, the drainage group showed decreased postoperative complications, including leakage of ascites, wound infection, and collection of ascites. Drainage by urostomy bag can prevent prolonged leakage of ascitic fl uid after the blockage of abdominal drains in patients undergoing cirrhotic hepatectomy.
abdominal drain;ascitic fl uid leak; hepatectomy; urostomy bag
Introduction
Abdominal drainage is a traditional procedure performed postoperatively. This procedure aims to detect postoperative intra-abdominal hemorrhage, remove bile leakage and debris, avoid subphrenic infection, and drain ascites, thus lowering abdominal tension.[1]The drainage catheter is usually removed at the end of the fi rst week after an operation. Increasing data have shown that routine placement of surgical drainage might induce a prolonged postoperative stay and/or decrease the rate of postoperative complications after abdominal operations including hepatectomy.[2-7]Besides, early removal (on postoperative day 2) of drainage tube based on a volume of drain discharge less than 450 mL could shorten signif i cantly the hospital stay without increase of complications.[8]Even in orthotopic liver transplantation, no data available to date indicate that routine abdominal drainage is useful.[9]Two randomized controlled studies recommended intraabdominal closed drainage in patients with cirrhosis undergoing hepatectomy for hepatocellular carcinoma, mainly if they present with preoperative portal vein thrombus or portal hypertension.[2,10]Cirrhotic hepatectomy, on the other hand, is mostly complicated by prolonged ascitic fl uid drainage from the abdominal drain.[11]Leakage of ascitic fl uid through the drain wound after drain cavity blockage or removal and subsequent development of a drain site wound infection and intraabdominal sepsis are commonly encountered if the abdominal drain is inserted through a straight tract.[12]The usual practice of suturing the skin of the drain site upon drain removal does not always go well. As a result, leakage of ascitic fl uid continues through the sutured wound site. Solutions to this postoperative complication remain elusive. Thus, a retrospective randomized studywas performed to compare suture ligation with urostomy bag drainage after abdominal drainage blockage following elective hepatectomy in patients with chronic liver disease.
Methods
Fifty-nine patients who had experienced leakage of ascites from their main wound or drain site after drain removal were divided into two groups: a suture group, in which suturing of the drain site or leakage site from the main abdominal wound was performed, and a drainage group, in which urostomy bags were placed to drain the leakage site. Patients with biliary anastomosis were excluded from this study, and the data set represented only those patients who had undergone resection of the hepatic parenchyma. Informed consent was obtained from all the patients, and the study protocol was approved by the ethics committee of our hospital.
In this study, the extent of hepatectomy was described in terms of Couinaud segments, whereas hepatectomy was def i ned as removal of three or more segments. Preoperative treatment was not applied. Parenchymal transection was performed by the crushing clamp method. Inclusion criteria for the patients in this study were a diagnosis with Child-Pugh A cirrhosis, a single hepatocellular carcinoma of less than 5 cm, and surgical resection as the fi rst-line treatment. Abdominal drainage consisted of two silicone rubber closed drains inserted through a separate stab incision and placed in the subdiaphragmatic and subhepatic spaces. Drains were removed after blockage. All patients received the same perioperative care by the same team of surgeons. Blockage of the abdominal drain with fresh clots was recorded for all patients (Fig.).
Statistical analysis was performed using the SPSS 12.0 software (SPSS, Chicago, IL., USA). The continuous variables were expressed as mean±SD. Differences in proportions were tested by the Chi-square test or Fisher's exact test. Comparisons of means between the two groups were tested by Student'sttest. Levene's test was used for the equality of variances.P<0.05 (twosided) was considered statistically signif i cant.
Results
In this series, 28 patients were included in the drainage group, whereas the other 31 in the suture group. Differences in demographic features were not found between the two groups (Table). And 56 (94.9%) patients were found to have a positive serological test for HBsAg.
All patients had a preoperative diagnosis of hepatocellular carcinoma that was conf i rmed histologically. They underwent major hepatectomy for three or more Couinaud segments. In-hospital death did not occur in each group. All the patients had their abdominal drain removed after blockage. The mean length of postoperative hospital stay in the drainage group was shorter than in the sutured group (16.11±2.61 vs 34.23 ± 4.86 days,P=0.000). Complications of the patients were compared after major hepatectomy. Leakage of ascites, wound infection, and collection of ascites were signif icantly differerent between the two groups (Table).
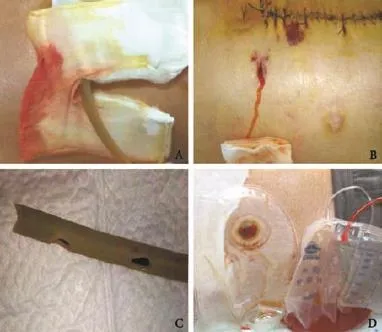
Fig.A 43-year-old man with hepatocellular carcinoma who underwent right trisegmentectomy (segments VI-VIII).A: Drain blockage on postoperative day 4;B: Ascitic fl uid from the drain site after drain removal;C: Silicone rubber closed drain blocked by fresh clots;D: Urostomy bag at the drain site.
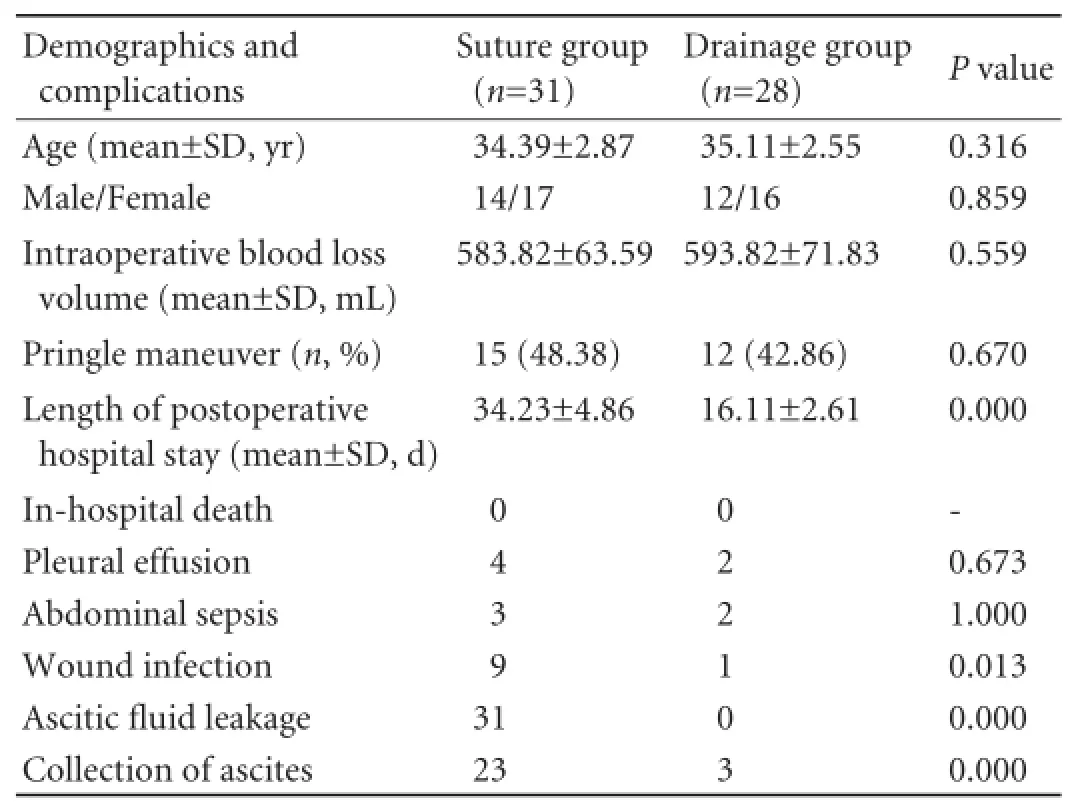
Table.Demographic characteristics and complications of the study samples
Discussion
One of the theoretical advantages of abdominal drainage in patients with chronic liver disease is the possibility of drainage of ascitic fl uid after hepatectomy to release the intra-abdominal pressure, resulting in improvement of postoperative abdominal distention and discomfort and minimizing splinting of the diaphragms. Current clinical practice suggests that routine use of a prophylactic drain is not necessary and early removal of the been-used drain is indicated. Reportedly, it is safer for minor hepatectomy without drainage, whereas the benef i ts of abdominal drainage in major hepatectomy are controversial.[12-14]Sun et al[15]recently reported that drainage is unnecessary when minor or major hepatectomy is performed using the crushing clamp method. However, due to the temporary deterioration of liver function after major hepatectomy, ascites formation is quite common in patients with cirrhosis. Our data indicate that abdominal drainage particularly benef i ts cirrhotic patients with preoperative portal hypertension, who are prone to develop liver decompensation and complications after surgery.
This investigation was conducted to review experience with drainage by urostomy bag placement after elective hepatectomy in our center. The data show that leakage of ascites after resection was less frequent among patients with a urostomy bag, although it did occur. Normal discharge from the drainage tube may provide a false sense of security if the tube has become blocked by the omentum or blood clots.[12]Blockage of the drainage catheter requires irrigation, and subphrenic infection would develop subsequently. Moreover, leakage will ensue because of the pressure of the ascitic fl uid that has built up in the peritoneal cavity. The usual practice of suturing the skin of the drain site after drain removal does not always turn out well. As a result, leakage of ascitic fl uid continues through the sutured site, which causes discomfort to patients. In the present study, suturing was found to increase complications, extend postoperative hospital stay, and result in higher medical expenses.
Use of a drainage tube after blockage was associated with a high incidence of local wound complications in this study. Especially common was leakage of ascites through the drainage wound, which has been associated with wound infection and abdominal sepsis. Despite the accumulation of ascites after hepatectomy, none of the patients in the drainage group developed any signif i cant ascitic fl uid leakage at the wound site or drain site after drain removal. In addition, wound infections were not observed at the drain insertion site in any of these patients. We consider drainage by urostomy bag placement a useful treatment modality after hepatectomy when an abdominal drain is blocked.
Contributors:WXH and SBC designed this experiment. All authors performed the operations. LGQ wrote this article. All authors read and approved the fi nal manuscript. SBC is the guarantor.
Funding:This study was supported by grants from the International Collaborational Foundation of Jiangsu Province (BZ2011041, ZX05200904 and WS2011106), and the National Nature Science Foundation of China (81100270 and 81070380).
Ethical approval:Not needed.
Competing interest:No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Merad F, Hay JM, Fingerhut A, Yahchouchi E, Laborde Y, Pélissier E, et al. Is prophylactic pelvic drainage useful after elective rectal or anal anastomosis? A multicenter controlled randomized trial. French Association for Surgical Research. Surgery 1999;125:529-535.
2 Hirokawa F, Hayashi M, Miyamoto Y, Asakuma M, Shimizu T, Komeda K, et al. Re-evaluation of the necessity of prophylactic drainage after liver resection. Am Surg 2011;77: 539-544.
3 Wang Z, Chen J, Su K, Dong Z. Abdominal drainage versus no drainage post gastrectomy for gastric cancer. Cochrane Database Syst Rev 2011;(8):CD008788.
4 Ishikawa K, Matsumata T, Kishihara F, Fukuyama Y, Masuda H, Kitano S. Laparoscopic cholecystectomy with and without abdominal prophylactic drainage. Dig Endosc 2011;23:153-156.
5 Liu HP, Zhang YC, Zhang YL, Yin LN, Wang J. Drain versus no-drain after gastrectomy for patients with advanced gastric cancer: systematic review and meta-analysis. Dig Surg 2011; 28:178-189.
6 Gurusamy KS, Samraj K, Mullerat P, Davidson BR. Routine abdominal drainage for uncomplicated laparoscopic cholecystectomy. Cochrane Database Syst Rev 2007;(4): CD006004.
7 Gurusamy KS, Samraj K, Davidson BR. Routine abdominal drainage for uncomplicated liver resection. Cochrane Database Syst Rev 2007;(3):CD006232.
8 Hayashi M, Hirokawa F, Miyamoto Y, Iwamoto M, Asakuma M, Shimizu T, et al. Optimal timing for removal of abdominal drainage after liver resection for hepatocellular carcinoma. Int Surg 2010;95:160-165.
9 Gurusamy KS, Naik P, Davidson BR. Routine drainage for orthotopic liver transplantation. Cochrane Database Syst Rev 2011;(6):CD008399.
10 Fuster J, Llovet JM, Garcia-Valdecasas JC, Grande L, Fondevila C, Vilana R, et al. Abdominal drainage after liver resection for hepatocellular carcinoma in cirrhotic patients: a randomized controlled study. Hepatogastroenterology 2004; 51:536-540.
11 Chan KM, Lee CF, Wu TJ, Chou HS, Yu MC, Lee WC, et al. Adverse outcomes in patients with postoperative ascites after liver resection for hepatocellular carcinoma. World J Surg 2012;36:392-400.
12 Lu L, Sun HC, Qin LX, Wang L, Ye QH, Ren N, et al. Abdominal drainage was unnecessary after hepatectomy using the conventional clamp crushing technique. J Gastrointest Surg 2006;10:302-308.
13 Kim YI, Hwang YJ, Chun JM, Chun BY. Practical experience of a no abdominal drainage policy in patients undergoing liver resection. Hepatogastroenterology 2007;54:1542-1545.
14 Kyoden Y, Imamura H, Sano K, Beck Y, Sugawara Y, Kokudo N, et al. Value of prophylactic abdominal drainage in 1269 consecutive cases of elective liver resection. J Hepatobiliary Pancreat Sci 2010;17:186-192.
15 Sun HC, Qin LX, Lu L, Wang L, Ye QH, Ren N, et al. Randomized clinical trial of the effects of abdominal drainage after elective hepatectomy using the crushing clamp method. Br J Surg 2006;93:422-426.Received June 10, 2012
Accepted after revision August 16, 2012
(Hepatobiliary Pancreat Dis Int 2013;12:99-102)
AuthorAff i liations:Liver Transplantation Center, First Aff i liated Hospital, Nanjing Medical University; Key Laboratory of Living Donor Liver Transplantation of Ministry of Public Health, Nanjing 210029, China (Li GQ, Zhang F, Lu H, Lu L, Li XC, Wang XH and Sun BC)
Bei-Cheng Sun, MD, PhD, Liver Transplantation Center, First Aff i liated Hospital, Nanjing Medical University, 300 Guangzhou Road, Nanjing 210029, China (Tel: 86-25-68136476; Fax: 86-25-86560946; Email: Sunbc@njmu.edu.cn)
? 2013, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(13)60013-2
 Hepatobiliary & Pancreatic Diseases International2013年1期
Hepatobiliary & Pancreatic Diseases International2013年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Terry's nail:an overlooked physical finding in cirrhosis
- Melanoma in the ampulla of Vater
- Hepatic portal venous gas in pancreatic solitary metastasis from an esophageal squamous cell carcinoma
- News
- TRAIL-induced expression of uPA and IL-8 strongly enhanced by overexpression of TRAF2 and Bcl-xL in pancreatic ductal adenocarcinoma cells
- Advantages of early cholecystectomy in clinical practice of a terciary care center
