Primary Sj?gren's Syndrome Accompanied by Intestinal Obstruction:a Case Report and Literature Review
Jie-ting Jia,Hua Wei*,and Hui Li
Department of Rheumatology,the Northern Jiangsu People's Hospital,Yangzhou 225001,China
SJ?GREN'S syndrome (SS) is a chronic inflammatory autoimmune disease characterized by the infiltration of lymphocytes and plasma cells in exocrine glands,especially salivary and lacrimal gland interstitium.The clinical manifestations of SS are complex.When the digestive system is involved,the patient always presents with liver damage,atrophic gastritis,and chronic diarrhea.Intestinal obstruction is rare and the specific pathogenesis remains unclear.1Currently,there is no clear treatment guidelines for SS with intestinal obstruction.The general measures include gastrointestinal decompression,spasmolysis,and other symptomatic treatments and the use of glucocorticoid to control the progressing of disease.Here we describe a case of primary SS with intestinal obstruction who was treated with conservative treatment.
CASE DESCRIPTION
A 36-year-old woman visited the Northern Jiangsu People's Hospital in October 2010 because of fever with fatigue for one month.Her temperature was approximately 37.5°C.Meanwhile,she had nausea and vomiting for one week.She was an housewife,and her family history was unremarkable.She had an appendicitis opepration when she was a teenager.Two months ago,she went to another hospital in Yangzhou to dissect the right cervical lymph node and the pathological report showed chronic inflammation with hyperplasia.A diagnosis of SS had been made 3 years before because of severe xerostomia and dry eyes,accompanied by recurrent parotid gland swelling.Anti-Ro/SSA and -La/SSB antibodies were both positive.Her vital signs were as follows:blood pressure 105/70 mm Hg,pulse rate 90/minute,respiration rate 20/minute,and body temperature 37.0°C.The patient was conscious and oriented.She appeared chronically ill and moderate pale.There was no erythema on her face and no oral ulcer either.She also had no decayed teeth or swelling parotid gland.Chest auscultation revealed no crackles or rhonchi in both lung fields;the heart sounds were normal too.The abdomen and extremities showed no abnormity and bowel sounds were 4 times/minute.
Laboratory test results showed a white blood cell count of 9.0 × 109/ L (neutrophil 65.8%),hemoglobin of 88 g/L,and platelet count of 97×109/ L. The urine protein was negative.The erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) were elevated to 125 mm/hour and 28.1 mg/L,respectively.The serum biochemal results,including globulin,alanine transpeptidase/aspartate aminotransferase,lactate dehydrogenase,and alkaline phosphatase values,were 46.7 g/L,16/33 U/L,584 U/L,and 167 U/L,respectively.The serum potassium ion was 3.07 mmol/L.Procalcitonin was 0.75 ng/mL.Antituberculin was negative.Bone marrow and blood cultures were both negative.However,the total protein was increased to 68.5 g/L and the albumin decreased to 31 g/L.These findings indicated a reversal of the albumin to globulin ratio.In addition,the blood urea nitrogen,creatinine,and the urine analysis were all within normal limits.The rheumatoid factor was high.Rheumatoid factor (RF)-IgG,RF-IgA,and RF-IgM were 68 U/mL,160 U/mL,and 94 U/mL,respectively.Anti-nuclear antibody was 1:1000.Anti-SSA antibody was positive and anti-SSB antibody was weakly positive.Anti-dsDNA,anti-nucleosome,anti-keratin,and anticardiolipin antibodies were all negative.IgG rose to 20.8 g/L while IgA and IgM remained normal.Liver-cytoplasm antigen was positive.Corneal erosions were noted in eye examination,along with a decrease in lacrimal secretions and tear break-up time being 2 seconds for both eyes.Salivary gland biopsy showed grade III-IV lymphocyte infiltration (Fig.1).Bone marrow slides showed reduced erythroid hyperplasia.The chest computed tomography (CT) showed bullae on left superior lung and lymph nodes in both sides of axillary fossa and mediastinum.
According to the 1997 recommended classification criteria for systemic lupus erythematosus (SLE),the data is insufficient for the diagnosis as SLE.After discussion,a diagnosis of primary SS was finally made.But the possibility of developing into other rheumatic diseases can not be ruled out,particularly SLE.
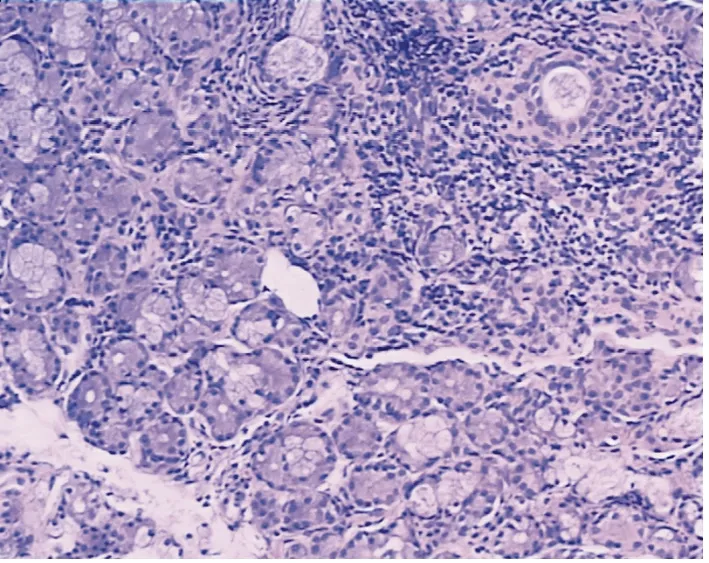
Figure 1.Histology of salivary gland showing grade III-IV lymphocyte infiltration,fibrosis,and slight acinar dilatation.HE ×100

Figure 2.Abdominal X-ray film before treatment (A) shows intestinal obstruction and dilated bowel,and the film after treament (B) demonstrates improvement.
Under the moderate glucocorticoid (methylprednisolone 24 mg/d) and immunosuppressant treatment,she had abdominal pains and distension,no passage of gas after 10 days.X-ray of the abdomen showed intestinal obstruction and dilated bowel (Fig.2A).She was then ordered to fast for 65 hours.Treatment was simultaneously given,including fluid replacement,maintenance of fluid and electrolyte balance,and active anti-infection treatment.Meanwhile,we increased the dose of glucocorticoid to 40 mg/d.Two days later,she felt better,but we still saw a small amount of liquid-gas levels in the X-ray.The blood routine test showed a white blood cell count of 14.1×109/ L,hemoglobin of 60 g/L,and platelet count of 77×109/ L.The blood direct Coombs' test result was positive and the count of reticulocyte was 0.284 × 1012/ L (ratio to 28.8%) .These results suggested that she had hemolytic anemia.The dose of methylprednisolone was raised to 240 mg/d for 3 days,then reduced to 80 mg/d.Her symptoms were relieved,she had passage of gas and stool,and no vomiting.Her bowel sounds were 3-4 times/minute.X-ray of the abdomen showed recovery.However,on the third day of methylprednisolone at 80 mg/d,the patient had vomiting and disappearance of bowel sounds again.Her ESR and CRP were 130 mm/hour and 0.14 mg/L,respectively.The plain and enhanced CT of abdomen showed no obvious abnormalities except enlarged spleen.The dose of glucocorticoid was adjusted to 240 mg/d again.Three days later,her symptoms and abdominal X-ray (Fig.2B) both got better and her hemoglobin increased to 78 g/L.Then she and her family demanded to go to Beijing for further treatment,where the same high-dose glucocorticoid therapy was performed.She was discharged 10 days later,and has visited our out-patient clinic for periodical check-ups up to now.At present,she received prednisone at 25 mg/d and hydroxychloroquine therapy,including hydroxychloroquine 0.2 g twice a day and total glucosides of paeony 0.6 g thrice a day.Her condition remained stable and has had no recurrence of intestinal obstruction so far.
DISCUSSION
Primary SS is a chronic autoimmune disease.There are two main categories of pathology of primary SS.First of all,there exists a large amount of lymphocyte infiltration,expansion,and stenosis of the gland duct in exocrine glands,which induce the epithelial cell proliferation,followed by degeneration,atrophy,destruction,and serious functional lesion.The other pathological feature is vasculitis due to cryoglobulinemia,high hypergammaglobulinemia,or deposition of immune complexes.There are inflammatory cells infiltrating around the vessel wall,and thrombosis and local tissue ischemia may occur.This disease occurs more in middle-aged women and the onset is mostly insidious.The etiology may involve genetics,viral infection,or endocrine factors.There is massive lymphocyte infiltration in the affected organs and a variety of autoantibodies in the serum of primary SS patients.The positive rates of anti-SSA and anti-SSB antibody are both higher than in other connective tissue diseases.1
The clinical symptoms of SS vary,and some patients do not present dry eyes or dry mouth,making it easy to misdiagnose.It may have multi-system involvement.In the respiratory system,it might be complicated by tracheitis,bronchitis,fibrosis alveolitis,interstitial pneumonia,atelectasis,pleurisy,and pleural effusion.About half of SS patients have concomitant kidney damage.The distal renal tubule acidosis accounts for 90% of the damage.SS may lead to hypokalemic periodic paralysis,renal chondropathy,and uropoiesis calculus.When the exocrine glands of gastrointestinal mucosa are damaged,atrophic gastritis,chronic diarrhea,and other non-specific symptoms would emerge.SS may also cause liver disease,which is mainly marked by hepatomegaly and liver function abnormalities.Chronic active hepatitis and primary biliary cirrhosis are common.1SS with intestinal obstruction is rare and the mechanism is not very clear.SS may lead to gastrointestinal mucosal atrophy,intestinal smooth muscle dysfunction,and topically insufficient blood supply,which is caused by vasculitis,weakening the gastrointestinal motility,followed by paralytic ileus.1In addition,some patients have antineutrophil cytoplasmic antibody (ANCA).ANCA can activate neutrophil degranulation,release proteases,activate toxic oxygen-derived free radicals,and increase nitric oxide.It also can ruin endothelial cells by directly binding to them.The patient in this report did not have ANCA.
There are few reports about primary SS with intestinal obstruction.In 1990,Adachi et al2reported one case of SS accompanied by chronic intestinal pseudo-obstruction(CIP).Zheng et al3reported one case of SS with CIP in 2005,the patient's myeloperoxidase ANCA was positive.Gao et al4reported a case of SS complicated by chronic diarrhea and intestinal obstruction.That patient also had tubulointerstitial lesions,which was improved by glucocorticoid therapy.
In rheumatic diseases,intestinal obstruction occurs most frequently in SLE5,6and systemic sclerosis (SSc).7-9And there are many examples for the latter.Haque et al7reported one case of scleroderma combined with volvulus.Osada et al8reported a SSc patient who had endoscopic duodenal stenosis.Meanwhile,that study proved that it had nothing to do with the use of non-steroid anti-inflammatory drugs.In a recent report,metronidazole was used to treat a case of SSc-associated pseudo-obstruction,producing a satisfactory outcome.9Except for the diffuse connective tissue diseases,intestinal obstruction can also be seen in ankylosing spondylitis.10
There is no special treatment for SS with intestinal obstruction,but early diagnosis is very important.The occurrence of intestinal obstruction suggests the necessity of timely measures.Glucocorticoid and immunosuppressive agents could be administered as the principle treatment.Moreover,symptomatic treatments are required to prevent the progress to intestinal necrosis and perforation,which include gastrointestinal decompression,maintaining homeostasis,and parenteral nutrition support.Because there is no clinical evidence of mechanical intestinal obstruction,surgery is invalid.Postoperative enteroparalysis would aggravate intestinal motor function.But once intestinal perforation or strangulation appears,an operation should be performed immediately to resect the necrotic bowel.
1.Edward DH,Ralph CB,Gary SF,et al.Kelley's textbook of rheumatology.Beijing:People's Health Publishing House;2006.p.944-55.
2.Adachi Y,Yabana T,Kohri T,et al.A case of chronic idiopathic intestinal pseudo-obstruction with Sj?gren's syndrome.Nihon Shokakibyo Gakkai Zasshi 1990;87:1223-7.
3.Zheng XJ,Gao M,Luo LH,et al.Chronic intestinal pseudo-obstruction in a patient with Sj?gren's syndrome.Chin J Intern Med 2005;44:667.
4.Gao M,Shen XL,Wang JG.Chronic diarrhea and intestinal obstruction in a patient with Sj?gren's syndrome.Chin J Intern Med 2006;45:594.
5.Tian XP,Zhang X.Gastrointestinal involvement in systemic lupus erythematosus:insight into pathogenesis,diagnosis and treatment.World J Gastroenterol 2010;16:2971-7.
6.Ceccato F,Salas A,Góngora V,et al.Chronic intestinal pseudo-obstruction in patients with systemic lupus erythematosus:report of four cases.Clin Rheumatol 2008;27:399-402.
7.Haque U,Yardley J,Talamini M,et al.Colon stricture and volvulus in a patients with scleroderma.J Rheumatol 1999;26:2268-72.
8.Osada T,Naqahara A,Ishikawa D,et al.Diaphragm-like stricture in the duodenum in a patient with systemic sclerosis:unrelated to non-steroidal anti-inflammatory drug use.Intern Med 2007;46:1697-700.
9.Azuma N,Nishioka A,Iizuka M,et al.Marked efficacy of metronidazole for the intestinal pseudoobstruction associated with systemic sclerosis.Nihon Rinsho Meneki Gakkai Kaishi 2011;34:53-61.
10.Zhang YW,Shen SJ,Cai H.Chronic intestinal pseudoobstruction in a patient with ankylosing spondylitis.Chin J Rheumatol 2008;5:358-9.
 Chinese Medical Sciences Journal2012年1期
Chinese Medical Sciences Journal2012年1期
- Chinese Medical Sciences Journal的其它文章
- Management of Pregnancy with Ankylosing Spondylitis
- Applicability of Community Periodontal Index Teeth and Random Half-mouth Examination to Gingival Bleeding Assessment in Untreated Adult Population in Beijing
- Personalized Management of Anastomotic Leak after Surgery for Esophageal Carcinoma
- Spectral Domain Optical Coherence Tomography of Vogt-Koyanagi-Harada Disease:Novel Findings and New Insights into the Pathogenesis
- Radiofrequency Ablation of Hepatic Paragonimiasis:a Case Report
- Electrocorticography with Direct Cortical Stimulation for a Left Temporal Glioma with Intractable Epilepsy
